Is It Snoring or Sleep Apnea?
I used to snore like hell!
It was so bad to the point that it affected my life.
I couldn’t go away with friends. If I went on a plane, I had to ensure I didn’t fall asleep.
It turned out I had severe obstructive sleep apnea. Maybe you do too, maybe not. In this article, I try to explore how you tell.

This is me on a recent flight to Europe with my travel CPAP machine.
Snoring is often considered a harmless annoyance, even cute if it’s a baby snoring. But sometimes it can be a symptom of a much more serious condition: sleep apnea. If you or a loved one snores loudly, it’s important to recognize when it’s just snoring and when it might be a sign of sleep apnea.
The good news is that detection has been made potentially easier with the introduction of apps and the new Apple iWatch 10. Not that I’ve tried any of these. But don’t take any of these devices or apps as a diagnosis. You should always see your medical professional if you think you have sleep apnea, where you will undergo a sleep study.
Let’s dig into the weeds and talk about the connection between snoring and sleep apnea.
In this guide, I’ll break down the differences, explain the risks, and discuss what steps you can take if you suspect sleep apnea might be at play.
What Is Snoring?
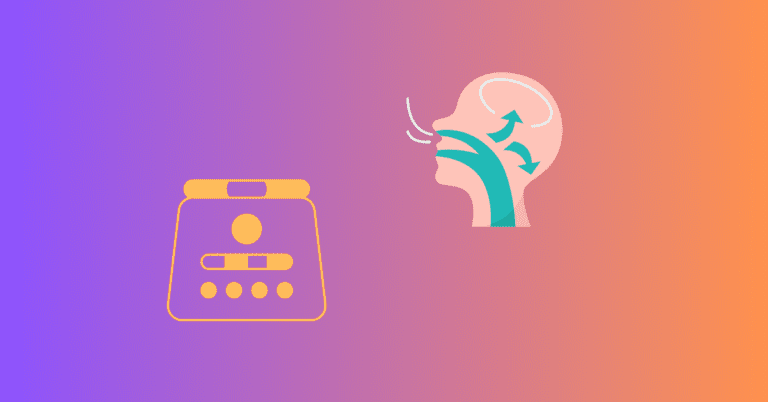
Snoring happens when the flow of air through the mouth and nose is partially blocked during sleep. This obstruction causes the surrounding tissues to vibrate, leading to that familiar snoring sound. Most people snore at some point in their lives, especially when they’re congested, after a night of drinking, or when sleeping in a specific position like on their back.
Factors that can contribute to snoring include:
- Sleeping Position: Lying on your back can cause the tongue to fall backward and partially block the airway.
- Nasal Congestion: Allergies, colds, or sinus infections can lead to snoring by narrowing the nasal passages.
- Alcohol or Sedative Use: These substances relax the muscles in the throat, making it more likely to snore.
- Obesity: Excess weight can increase fat tissue around the neck, causing airway constriction.
While snoring can be entirely benign, for some people, it’s a symptom of something more dangerous.
Personal Insight. For years, I thought my loud snoring was normal, especially since it only seemed to happen when I slept on my back. My family joked about how loud it was, but I never thought it could be a sign of something more serious. It also stopped me for doing things I would enjoy, like going traveling. It wasn’t until I started getting persistent migraines that I realized my snoring might be connected to a bigger problem.

What Is Sleep Apnea?
Sleep apnea, specifically obstructive sleep apnea (OSA), is a sleep disorder where your breathing repeatedly stops and starts throughout the night. Each pause in breathing, known as an apnea, can last anywhere from a few seconds to over a minute. These interruptions can happen hundreds of times per night, disrupting the sleep cycle and preventing you from reaching restorative, deep sleep stages.
In OSA, the muscles in the throat relax too much during sleep, causing the airway to collapse.
When the brain realizes that breathing has stopped, it sends signals to the body to wake up briefly and resume breathing.
This cycle can happen without the person even being aware, although they may notice frequent waking, gasping for air, or choking sensations. Unlike occasional snoring, OSA can lead to serious health problems if left untreated, such as:
- High Blood Pressure: Repeated drops in oxygen levels strain the cardiovascular system.
- Heart Disease and Stroke: OSA is linked to a higher risk of heart attacks and strokes due to chronic oxygen deprivation and increased blood pressure.
- Diabetes: There is a strong correlation between sleep apnea and insulin resistance, which can lead to type 2 diabetes.
- Daytime Fatigue: Sleep apnea sufferers often experience excessive daytime sleepiness, which can lead to poor concentration, memory problems, and even dangerous situations like falling asleep while driving.
Personal Insight: I never thought snoring could be dangerous, but over time, I started waking up gasping for air and feeling like I hadn’t slept at all.
My morning headaches and migraines were becoming more frequent, and it got to the point where I thought something more serious was going to happen to me.
I finally saw a doctor, took a sleep study and was diagnosed with severe obstructive sleep apnea.
Key Differences: How Can You Tell if It’s Just Snoring or Sleep Apnea?
While snoring and sleep apnea can overlap, some key symptoms may indicate whether your snoring is a harmless quirk or a sign of a more serious sleep disorder. Here are some questions to help you assess the situation:
- Is your snoring loud and persistent? Occasional, soft snoring may not be concerning, but if you or your partner notice loud, habitual snoring, it might be worth investigating further.
- Do you stop breathing during sleep? One of the hallmarks of sleep apnea is the cessation of breathing for brief periods. If your partner has noticed you stop breathing or wake up choking or gasping for air, it could be a sign of OSA.
- Do you wake up tired despite a full night’s sleep? Even if you get 7–9 hours of sleep, OSA can prevent you from reaching the deeper stages of sleep, leaving you exhausted during the day.
- Do you experience morning headaches or dry mouth? People with OSA often wake up with headaches due to oxygen deprivation during sleep. A dry mouth can also be a sign of mouth breathing caused by restricted airflow.
- Do you fall asleep during the day? People with OSA often struggle with daytime drowsiness, which can be dangerous in certain activities like driving or operating machinery.
If you experience any of these symptoms, it’s essential to consult a healthcare provider who can recommend a sleep study to confirm the diagnosis.
Personal Insight: At first, I didn’t think much of my snoring, but as I said, I started waking up with intense headaches every morning. I felt sluggish all day, and I couldn’t figure out why.
It wasn’t until my wife mentioned that I sometimes stopped breathing at night that I realized my snoring was more than just an annoyance.
Risk Factors for Sleep Apnea
Certain factors increase your risk of developing obstructive sleep apnea, even if you don’t currently have the condition. These include:
- Excess Weight: Obesity is one of the most significant risk factors for sleep apnea. Fat deposits around the neck can obstruct the airway during sleep.
- Large Neck Circumference: A neck size of over 17 inches in men and 16 inches in women is linked to an increased risk of OSA, as it can narrow the airway.
- Aging: As we get older, the muscles in our throat naturally lose some of their tone, which can contribute to airway collapse during sleep.
- Gender: Men are twice as likely as women to have OSA, although the risk increases for women after menopause.
- Family History: If other members of your family have sleep apnea, your risk of developing it is higher.
- Alcohol, Smoking, and Sedatives: All of these relax the muscles in the throat, increasing the chances of airway obstruction.
- Nasal Congestion: Chronic nasal congestion or other airway blockages can make it more difficult to breathe while sleeping, leading to snoring and sleep apnea.
Personal Insight: When I was diagnosed with severe sleep apnea, I wasn’t surprised to learn that my weight and neck size were major factors contributing to my condition. For this reason, I started to exercise more and join a gym. The good news was that I lost 22 pounds, the bad news was my sleep apnea still persists,
How Is Sleep Apnea Diagnosed?
The only way to definitively diagnose sleep apnea is through a sleep study, which can be conducted either in a sleep lab (polysomnography) or at home (home sleep apnea test). A sleep study measures various factors, including:
- Breathing patterns
- Oxygen levels
- Brain activity
- Heart rate
- Body movements
During the test, the number of apneas (breathing pauses) and hypopneas (shallow breathing) you experience per hour is recorded. This is known as the Apnea-Hypopnea Index (AHI), and it helps classify the severity of sleep apnea.
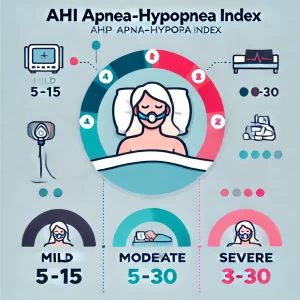
- Mild Sleep Apnea: AHI of 5-15 events per hour
- Moderate Sleep Apnea: AHI of 15-30 events per hour
- Severe Sleep Apnea: AHI of over 30 events per hour
Once diagnosed, your doctor will discuss treatment options, which may include CPAP therapy, lifestyle changes, or other medical interventions.
Personal Insight: When I did my sleep study, the results were shocking. I was having over 40 breathing interruptions per hour! I didn’t realize how badly my sleep was being affected until I saw the data. That’s when I knew I needed to take action.
Treatment Options for Sleep Apnea
If you’ve been diagnosed with obstructive sleep apnea, there are several treatment options available depending on the severity of your condition:
- Continuous Positive Airway Pressure (CPAP): CPAP therapy is the most common and effective treatment for OSA. It involves wearing a mask over your nose or mouth while you sleep, which delivers constant air pressure to keep your airways open.
- Lifestyle Changes: In some cases, weight loss, quitting smoking, and avoiding alcohol or sedatives before bed can reduce the severity of sleep apnea.
- Oral Appliances: For mild to moderate sleep apnea, a custom-fitted mouthpiece may help keep your airway open by repositioning the jaw and tongue during sleep.
- Surgery: In severe cases where other treatments are ineffective, surgery may be considered to remove excess tissue, reposition the jaw, or insert implants to support the airway.
Personal Insight: Using a CPAP machine has been life-changing for me. It took a little while to get used to, but now I sleep so much better, and my energy levels during the day have improved dramatically.
It’s amazing how much of a difference it makes when your body is finally getting the oxygen it needs.

Conclusion
Snoring may seem like a minor inconvenience, but it could be a sign of something much more serious: sleep apnea.
Recognizing the difference between simple snoring and obstructive sleep apnea is crucial for your health. If you’re concerned about your snoring, don’t hesitate to seek medical advice—early diagnosis and treatment can significantly improve your quality of life.
Personal Insight: Looking back, I’m so glad I didn’t ignore the signs. My loud snoring was more than just an annoyance—it was a warning that my health was at risk. Getting diagnosed with sleep apnea and starting CPAP therapy has changed my life, and I feel like a new person with so much more energy and focus.