AHI Apnea-Hypopnea Index – What You Need to Know
Jeremy Smith is a long-term CPAP user and sleep apnea advocate. After being diagnosed with severe obstructive sleep apnea, he created ByJeremySmith.com to help others navigate CPAP therapy through personal stories, gear reviews, and practical advice.
Sleep apnea is more than just a sleep disorder—it can severely impact daily life, energy levels, and overall health.

As someone who has experienced the debilitating effects of severe obstructive sleep apnea, I know firsthand how important it is to get an accurate diagnosis. When I was first diagnosed, I felt completely drained every day without understanding why.
It wasn’t until my at-home CPAP sleep study revealed a sky-high AHI Apnea-Hypopnea Index (AHI) score that I fully grasped what was happening. That diagnosis changed everything for me, especially once I began CPAP therapy.
In this article, I’ll explain the AHI, how it’s calculated, and why it’s crucial for diagnosing and treating sleep apnea.
My journey with severe sleep apnea taught me that understanding your AHI score is the first step toward reclaiming your health and energy.
What Is the AHI Apnea-Hypopnea Index?
The Apnea-Hypopnea Index (AHI) is a scale used to measure the number of times a person’s breathing is either fully or partially obstructed during sleep. These interruptions in breathing are classified as either apneas (complete cessation of airflow for at least 10 seconds) or hypopneas (partial reductions in airflow for at least 10 seconds).
The AHI score represents the average number of these events per hour of sleep. The higher your AHI score, the more severe your sleep apnea.
In my case, my sleep study revealed a shockingly high AHI score, which made it clear just how severe my obstructive sleep apnea was. It was this diagnosis that led me to start CPAP therapy, which has since transformed my quality of life.
How Is the AHI Calculated?
The AHI score is determined through a sleep study or polysomnography. During the study, sensors are placed on your body to monitor your breathing patterns, oxygen levels, heart rate, and brain activity while you sleep.
The data collected is used to calculate how often apneas and hypopneas occur during your sleep cycle.
Here’s a simple breakdown of the AHI formula:
- AHI = (Number of Apneas + Number of Hypopneas) / Total Hours of Sleep
For example, if you had 50 apneas and hypopneas during a 5-hour sleep period, your AHI score would be:
- AHI = 50 / 5 = 10
This AHI score falls within the mild sleep apnea range, which we’ll explore in more detail below.
What Do AHI Scores Mean?
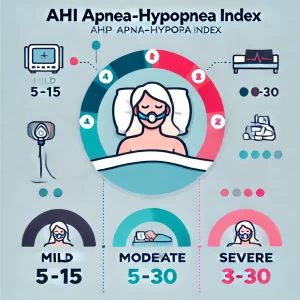
The AHI score is classified into different categories of sleep apnea severity:
- Normal (AHI < 5): Less than 5 events per hour are considered normal, and no treatment may be necessary.
- Mild Sleep Apnea (AHI 5-15): 5 to 15 events per hour indicate mild sleep apnea. This was the level at which I first began noticing my excessive daytime fatigue and snoring, but I didn’t initially realize it was linked to my breathing during sleep.
- Moderate Sleep Apnea (AHI 15-30): 15 to 30 events per hour indicate moderate sleep apnea. Symptoms like snoring, waking up gasping for air, and frequent nighttime awakenings become more noticeable.
- Severe Sleep Apnea (AHI 30+): More than 30 events per hour indicate severe sleep apnea. This was my diagnosis, with over 30 interruptions every hour. No wonder I was always exhausted and struggling to stay focused during the day!
When I received my diagnosis, my AHI score was well into the severe range, which explains why I felt so drained all the time.
But more importantly, it gave me an understanding of what was happening to my body and allowed my doctor to develop an effective treatment plan.
Why Is the AHI Important?
The AHI score is crucial because it objectively measures how severely your breathing is disrupted during sleep.
This number helps doctors determine the severity of your sleep apnea and the most appropriate course of treatment.
Here’s why understanding your AHI score matters:
- Treatment Decisions: Your AHI score guides your doctor in choosing the right treatment. For mild cases, lifestyle changes or an oral appliance might be sufficient. For moderate to severe cases, CPAP therapy is usually recommended.
- Health Implications: Untreated sleep apnea, particularly with a high AHI score, can lead to serious health issues like high blood pressure, heart disease, stroke, and type 2 diabetes. Knowing your AHI score helps you understand the urgency of getting treatment.
- Tracking Progress: After starting treatment, such as CPAP therapy, your doctor may use follow-up sleep studies to check if your AHI score has improved, helping to adjust your treatment plan if needed.
In my case, starting CPAP therapy had a dramatic effect on my AHI score.
Within a few weeks of regular use, my AHI dropped significantly, and I began to feel like a new person—more energized, alert, and able to focus during the day. Seeing how the numbers correlated with real changes in how I felt was incredible.
When I look at the AHI number on my machine in the morning, it’s around 2 to 4 events per hour. Sometimes as low as 1, which is fantastic.
AHI and CPAP Therapy: How It Changes Lives
For those of us diagnosed with obstructive sleep apnea, a CPAP machine (Continuous Positive Airway Pressure) is usually prescribed. This device keeps the airway open by delivering a constant stream of air pressure, preventing the blockages that lead to apneas and hypopneas.
When I first started using CPAP, it was a bit of an adjustment—sleeping with a mask on wasn’t exactly comfortable at first. But the benefits far outweigh any initial discomfort. As my AHI score improved, I noticed huge changes in my life:
- No more Migranies: I swear, these were killing me. Now they have totally gone away 🙂
- Better Sleep Quality: I no longer woke up gasping for air, and my sleep became more restful.
- Increased Energy: My daytime fatigue disappeared, and I started waking up feeling refreshed and ready to take on the day.
- Improved Focus: Before CPAP, I struggled with brain fog and difficulty concentrating. After treatment, I felt sharper and more mentally clear.
The improvement in my AHI score was a tangible sign that the therapy was working and motivated me to stick with it. I could see the difference in the data, but more importantly, I could feel the difference in my body and mind.
Other Factors That Affect the AHI Score
While the AHI is an essential tool for diagnosing and treating sleep apnea, it’s important to remember that it’s not the only factor your doctor will consider.
Other aspects of your health can influence the severity of your sleep apnea and may need to be addressed as part of your treatment plan.
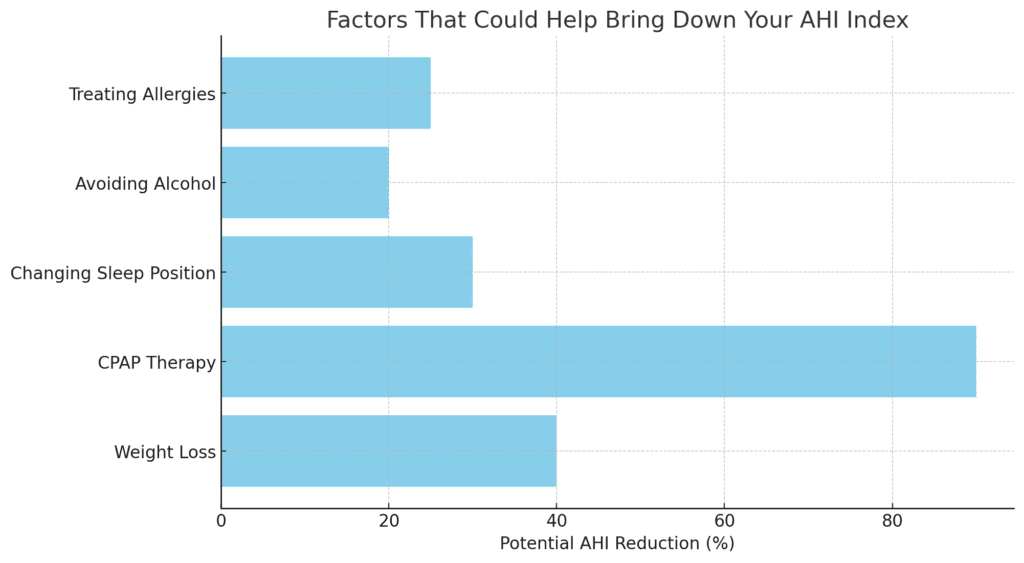
- Weight: Obesity is one of the biggest risk factors for sleep apnea. Losing weight can help reduce the severity of sleep apnea and lower your AHI score.
- Age: Sleep apnea is more common as people get older, as the muscles in the throat naturally weaken with age.
- Neck Circumference: A thicker neck can narrow the airway, increasing the likelihood of blockages.
- Sleeping Position: Sleeping on your back can worsen sleep apnea, as gravity makes it easier for your airway to become blocked.
In my case, I worked with my doctor to make lifestyle changes, including losing some weight and adjusting my sleeping position, which helped further improve my sleep and AHI score.
Conclusion: Why Knowing Your AHI Score Matters
Understanding the AHI Apnea-Hypopnea Index is key to managing sleep apnea effectively. Whether you’ve been diagnosed with mild, moderate, or severe sleep apnea, knowing your AHI score allows you and your healthcare provider to develop a tailored treatment plan that can significantly improve your quality of life.
For me, learning about my AHI score was the turning point that led to a diagnosis and treatment that truly changed my life.
Thanks to CPAP therapy and lifestyle adjustments, I’m sleeping better, feeling more energetic, and living healthier. If you suspect you may have sleep apnea, don’t wait—seek out a sleep study and determine your AHI score. It could be the first step toward a better, more rested version of yourself.
Do you have any questions about the AHI Apnea-Hypopnea Index? If so, please let me know in the comments section below.
Disclaimer: The content on this blog is for informational and educational purposes only and is not a substitute for professional medical advice. Always speak with your doctor or sleep specialist before starting, stopping, or changing any treatment or therapy related to sleep apnea or CPAP use.