CPAP Sleep Study – What to Expect from a Polysomnography Test
If you’re waking up groggy, snoring like a freight train, or dozing off as soon as you hit the couch, a CPAP sleep study—specifically, an in-lab polysomnography—might be your turning point.

I’ve been there. Years of brain fog, daytime exhaustion. I even dodged going to camp when I was young cause I knew more snoring would annoy everyone and probably get me kicked!
I had no clue I was waking up dozens of times an hour, and it was having a tremendous negative impact on my heart. My sleep study changed everything. It led to my CPAP prescription, which has been life-saving.
Let’s walk through what a CPAP sleep study is, how it works, and how it could change your life, too.
What Is a CPAP Sleep Study?
A polysomnography (PSG) is a comprehensive overnight test that measures your brain waves, breathing, heart rate, oxygen levels, and muscle activity while you sleep. It’s often the first step toward diagnosing obstructive sleep apnea and determining whether you’ll benefit from CPAP therapy.
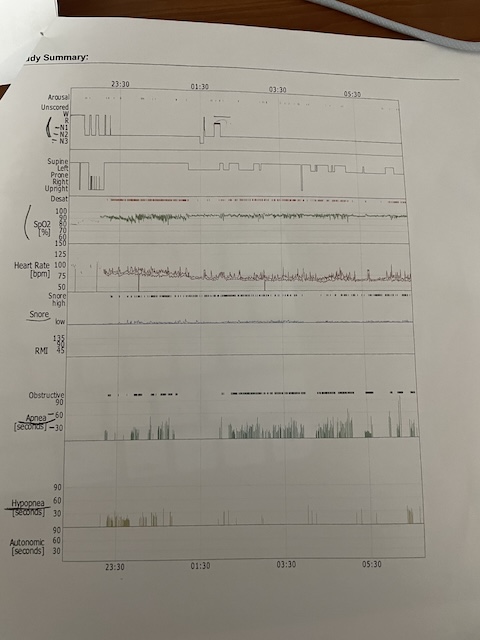
These are my results.
The technician has pointed to the 60 as my apneas are hitting this number. 60 an hour or one apnea every minute, which is interpreted as severe.
PSGs are typically done in a sleep lab under the supervision of a trained technician. This isn’t the same as a home test (called HSAT)—those are simpler and only capture limited data.
The National Library of Medicene has a comprhernsive beak down of what you can expect during a polysomnography and what is measured.
In-lab sleep studies can detect not just sleep apnea, but also:
- Periodic limb movement disorder
- REM behavior disorder
- Narcolepsy
- Central sleep apnea
How Polysomnography Works (And Why It’s So Valuable)
Think of it like a full-body scan while you sleep. You show up in the evening, and a technician gently applies sensors to your scalp, chest, legs, and face. Yes, you’ll be wired up—but the goal is to capture as much data as possible.
These sensors track:
- Brain waves (EEG)
- Eye movement (EOG)
- Muscle tone (EMG)
- Heart rate and rhythm (ECG)
- Breathing effort and airflow
- Oxygen saturation
They also use video monitoring and a microphone to capture snoring or gasping.
What to Expect During the Night
You’ll arrive a couple of hours before bedtime. The room feels like a hotel—quiet, private, comfortable. Once you’re wired up, the tech will monitor your signals from a separate room.
If moderate to severe sleep apnea is suspected, your study might become a split-night test: the first half diagnoses the apnea, and the second half tests you on CPAP. This part is called titration—adjusting pressure levels until apneas are eliminated.
💡 Want the deep dive? Check out my full post on CPAP titration.
What the Sleep Study Reveals
Your results might look like alphabet soup, but here’s what matters most:
- AHI (Apnea-Hypopnea Index): Number of breathing interruptions per hour. 30+ means severe apnea.
- ODI (Oxygen Desaturation Index): Tracks how often your oxygen drops below normal.
- Sleep Staging: How much time you spend in light, deep, and REM sleep.
- Arousals & Fragmentation: Shows how often your brain wakes up—even if you don’t remember it.
For me, these numbers were shocking. I was having around 60 breathing events an hour. No wonder I felt like a zombie. I was shocked, but on the other hand, it explained years of snoring, sore throats, headaches, and migraines, which were getting more frequent.
What Does Healthy Sleep Look Like?
Your sleep is divided into stages: light sleep, deep sleep (N3), and REM. A typical night cycles through these stages 4–6 times.
- N1 & N2 (Light Sleep): Makes up ~50% of your night. You’re easy to wake, but still resting.
- N3 (Deep Sleep): Crucial for physical recovery, immune health, and cellular repair.
- REM Sleep: Where most dreaming happens. Important for mood, memory, and learning.
A sleep study shows how often you enter each stage—and whether apneas are preventing deeper, restorative sleep. In my case, I was stuck in light sleep all night, waking up feeling like I hadn’t slept at all.
What If They Put You on CPAP That Night?
If your apnea is moderate to severe, your PSG might become a split-night study. That means you’ll sleep the first half without CPAP, and the second half with a CPAP machine on.
This allows the technician to adjust your air pressure in real-time to find the lowest level that eliminates apneas. It’s called a CPAP titration.
Don’t worry—this isn’t trial by fire. Most labs have a range of masks (nasal pillows, nasal masks, full face) and the technician will help you find one that fits. Some labs even use heated tubing and humidifiers to improve comfort.
When I had my first night on CPAP, I was shocked. I woke up alert for the first time in years. That single night sold me on the therapy.
👉 Curious about titration in depth? Read What Is CPAP Titration?
The other type of sleep study you can do is a home-based sleep study. It’s a lot less intimidating, and might be your only option depending on where you live. It’s also a lot cheaper!
Here’s a quick comparison…
Polysomnography vs. Home Sleep Test (HSAT)
| Feature | In-Lab PSG | Home Sleep Test (HSAT) |
|---|---|---|
| Tracks Brain Activity | ✅ Yes | ❌ No |
| Captures Full Sleep Staging | ✅ Yes | ❌ No |
| Technician Support | ✅ Yes | ❌ No |
| Comfortable Environment | ❌ Less so | ✅ Home |
| Cost | 💲💲💲 | 💲 |
| Best For | Complex or Severe Cases | Mild/Moderate, Low-Risk Cases |
💡 If you want a guide on HSATs, visit At-Home Sleep Apnea Test
When Should You Get a Sleep Study?
You might need a study if you:
- Snore loudly
- Wake up gasping or choking
- Feel tired despite 7–9 hours of sleep
- Have morning headaches
- Struggle with focus or memory
- Have high blood pressure or AFib
For me, it was my partner’s complaints that pushed me to get help. She said I stopped breathing in my sleep. Scary—but I’m grateful she noticed.
What to Bring to Your Sleep Study
Pack like you’re going to a hotel. Here’s what I recommend:
- Comfortable pajamas or loose-fitting sleepwear
- Your favorite pillow (yes, really!)
- Toiletries: toothbrush, face wash, etc.
- Book or phone for winding down
- A change of clothes for the next morning
- Health insurance card and referral paperwork
Bonus tip: Avoid caffeine after 2 p.m. and skip naps the day of your study.
What If My Sleep Study Doesn’t Show Anything?
It happens. Maybe you didn’t sleep long enough. Maybe apnea didn’t show up that night. If your results are borderline or unclear, your doctor may:
- Repeat the PSG on another night
- Try a home sleep apnea test (HSAT) for comparison
- Order a Multiple Sleep Latency Test (MSLT) to check for narcolepsy
Sleep isn’t always predictable, and one night doesn’t tell the whole story. Be patient with the process—it’s worth getting right.
Cost & Insurance Coverage
- In-lab sleep study: $1,000–$3,000 (before insurance)
- HSAT: $300–$600
Most insurance plans, including Medicare, cover diagnostic sleep studies when ordered by a doctor.
Even if there’s some out-of-pocket cost, the long-term health payoff is priceless.
What Happens After the Study?
Once your results are analyzed, your sleep specialist may recommend:
- CPAP therapy
- Further testing (like a titration night or MSLT)
- Lifestyle changes (weight loss, sleep positioning, etc.)
In my case, I started CPAP right after my titration. The change was immediate—I had energy again, my brain worked, and my relationship improved. Totally worth it.
FAQ
Is a CPAP sleep study uncomfortable?
It’s a little weird at first, but most people fall asleep faster than they expect. The rooms are private, and techs try to make you comfortable.
Can I bring my own pillow or pajamas?
Absolutely—and it helps! Familiar items make the environment feel less clinical.
What if I can’t sleep during the test?
They only need a few hours of quality data. And if needed, a repeat study can be done.
Can I go to work the next day?
Yes, though you may be a bit tired. If your test includes daytime nap studies (like MSLT), you’ll need to stay longer.
Will I need CPAP for life?
Not always. Some people improve with weight loss or surgery. But for many of us, CPAP is the safest, most effective long-term option.
Conclusion
A CPAP sleep study might sound intimidating, but it could be the best night of “sleep” you’ve had in years—because it leads to answers.
Polysomnography gave me the diagnosis that changed my life. If you’re struggling with exhaustion or unexplained symptoms, don’t wait.
📌 Next up: What Is CPAP Titration?
📌 Also explore: At-Home Sleep Apnea Test
⚠️ MEDICAL DISCLAIMER This blog provides general information only and is not a substitute for professional medical advice, diagnosis, or treatment. Sleep apnea is a serious condition, and CPAP equipment should be used under proper medical supervision. Always consult your doctor or sleep specialist before starting, stopping, or changing any therapy. I share personal experiences as a CPAP user, not as a medical professional. Individual results vary. For medical guidance, please consult a qualified clinician or the American Academy of Sleep Medicine (aasm.org).




