Overlap Syndrome: The Link with COPD and OSA
Overlap syndrome is a condition in which a person has both chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea (OSA).
This combination of two severe respiratory disorders can lead to worsened symptoms, increased health risks, and challenges in treatment.
If left unmanaged, overlap syndrome can severely impact sleep quality, lung function, and overall well-being.
In this article, we’ll explore overlap syndrome, its development, symptoms, and treatment options.
What Is COPD?
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that makes breathing difficult. It includes conditions like chronic bronchitis and emphysema, where the airways become narrowed, inflamed, or damaged, leading to airflow obstruction. COPD is often caused by long-term exposure to irritants, such as cigarette smoke, air pollution, or chemical fumes.
Symptoms of COPD include:
- Chronic cough.
- Shortness of breath, especially during physical activity.
- Wheezing.
- Excess mucus production.
- Frequent respiratory infections.
COPD affects millions of people worldwide and is a leading cause of respiratory disability.
What Is Obstructive Sleep Apnea (OSA)?
Obstructive sleep apnea (OSA) is a sleep disorder in which the airway becomes partially or completely blocked during sleep, causing repeated pauses in breathing (apneas). These interruptions can occur multiple times throughout the night, preventing the individual from reaching deep, restorative sleep. OSA is often associated with loud snoring, choking, or gasping sounds during sleep, and it can lead to excessive daytime sleepiness, fatigue, and an increased risk of cardiovascular disease.
Symptoms of OSA include:
- Loud snoring.
- Gasping or choking during sleep.
- Excessive daytime sleepiness.
- Difficulty concentrating.
- Morning headaches.
OSA is a common sleep disorder that affects millions of people worldwide and is often associated with obesity, but it can affect individuals of all body types.
What Is Overlap Syndrome?
Overlap syndrome occurs when a person is diagnosed with both COPD and OSA.
While these conditions affect breathing in different ways—COPD impacts lung function and airflow, and OSA involves airway blockages during sleep—having both conditions can lead to complex symptoms and heightened health risks.
People with overlap syndrome often experience more severe respiratory issues than those with just COPD or OSA alone.
The combination of these two disorders can lead to frequent drops in oxygen levels during sleep, a condition known as nocturnal hypoxemia, which can strain the heart and other organs.
Why Is Overlap Syndrome Dangerous?
- Frequent Oxygen Drops: Both COPD and OSA contribute to low blood oxygen levels. In OSA, the airway is blocked during sleep, and in COPD, the lungs struggle to exchange oxygen effectively. Together, these conditions can result in more pronounced oxygen desaturation at night.
- Increased Risk of Heart Disease: Overlap syndrome increases the risk of developing cardiovascular issues, such as high blood pressure, heart failure, and stroke. The frequent drops in oxygen levels strain the heart, leading to further complications.
- Worsened COPD Symptoms: Sleep disruptions from OSA can exacerbate COPD symptoms, leading to more frequent COPD flare-ups or exacerbations.
Symptoms of Overlap Syndrome
The symptoms of overlap syndrome are a combination of those associated with both COPD and OSA. However, the interaction of these conditions can lead to more severe or frequent respiratory difficulties, especially during sleep.
Symptoms may include:
- Worsened shortness of breath during the day and night.
- Frequent awakenings due to difficulty breathing.
- Morning headaches from low oxygen levels during the night.
- Excessive daytime fatigue and sleepiness due to interrupted sleep.
- Loud snoring and gasping for air during sleep.
- Increased mucus production and chronic coughing.
Patients with overlap syndrome may also experience more frequent hospitalizations due to COPD exacerbations or respiratory infections.
Diagnosing Overlap Syndrome
Diagnosing overlap syndrome requires a combination of tests to evaluate both sleep quality and lung function. These include:
Polysomnography (Sleep Study)
A polysomnography is a comprehensive sleep study that monitors various physiological parameters while you sleep, such as breathing patterns, oxygen levels, heart rate, and brain activity. It can detect the presence and severity of OSA by measuring how often apneas and hypopneas (shallow breathing) occur during the night.
Pulmonary Function Tests (PFTs)
To assess the severity of COPD, doctors use pulmonary function tests (PFTs) to measure lung capacity, airflow, and oxygen exchange. These tests help determine how well the lungs function and whether COPD contributes to the patient’s breathing difficulties.
Nocturnal Oximetry
A nocturnal oximetry test measures blood oxygen levels overnight to detect nocturnal hypoxemia. This test helps identify whether oxygen levels drop significantly during sleep, a key feature of overlap syndrome.
By combining the results of these tests, doctors can diagnose overlap syndrome and develop a comprehensive treatment plan.
Treatment Options for Overlap Syndrome
Treating overlap syndrome requires addressing both COPD and OSA to improve breathing during the day and night. Treatment options may include:
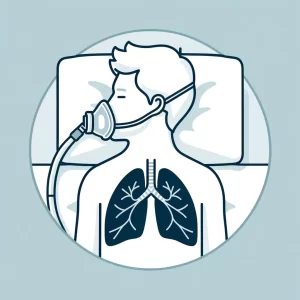
CPAP or BiPAP Therapy
CPAP (Continuous Positive Airway Pressure) or BiPAP (Bilevel Positive Airway Pressure) therapy is commonly recommended for the OSA component of overlap syndrome. CPAP delivers a continuous stream of air to keep the airway open during sleep. At the same time, BiPAP provides two levels of pressure, one for inhalation and one for exhalation, making it easier for people with COPD to breathe out.
Oxygen Therapy
For patients with severe COPD and nocturnal hypoxemia, oxygen therapy may be prescribed to ensure adequate oxygen levels are maintained during sleep. This therapy is often used alongside CPAP or BiPAP to prevent dangerous drops in oxygen levels.
Bronchodilators and Inhalers
To manage COPD symptoms during the day, doctors often prescribe bronchodilators or inhalers to help open the airways, reduce inflammation, and improve lung function. These medications can help reduce the frequency of COPD flare-ups and improve overall breathing.
Lifestyle Changes
Managing overlap syndrome also involves making lifestyle changes that can improve lung function and reduce sleep apnea symptoms, such as:
- Quitting smoking is one of the most essential steps for improving COPD.
- Losing weight, as obesity, can worsen OSA.
- Exercising regularly strengthens the respiratory muscles and improves lung capacity.
Seeking Help from Your Doctor
If you have COPD and suspect you might also have sleep apnea, it’s crucial to seek help from your doctor. Overlap syndrome can lead to serious health complications if left untreated, but with proper management, you can improve your quality of life and reduce the risks associated with both conditions.
A sleep specialist and pulmonologist can work together to diagnose overlap syndrome and develop a tailored treatment plan to address your unique needs. Managing both conditions is key to better health, whether through CPAP, oxygen therapy, or lifestyle changes.