Sleep Apnea Surgery: Procedures, Risks, and Outcomes
Jeremy Smith is a long-term CPAP user and sleep apnea advocate. After being diagnosed with severe obstructive sleep apnea, he created ByJeremySmith.com to help others navigate CPAP therapy through personal stories, gear reviews, and practical advice.
Sleep Apnea surgery might be the answer to your sleep apnea diagnosis if you don’t like the thought of using a CPAP machine for the rest of your life.
While Continuous Positive Airway Pressure (CPAP) therapy is the most common treatment, some people find it uncomfortable or ineffective.

I am one of these people. I used a CPAP machine for my obstructive sleep apnea, and it has truly worked miracles for my health.
But I know that some people can’t tolerate CPAP or want a more permanent solution. For these people, surgery could be an option.
This article will explore the various surgical treatments available for sleep apnea, their effectiveness, risks, and considerations.
What Is Sleep Apnea Surgery?
Sleep apnea surgery involves surgical intervention to improve airflow by altering the structure of the airway.
These procedures aim to reduce airway obstructions, which cause breathing pauses during sleep.
Depending on the severity of the apnea and the patient’s overall health, surgical options can range from minimally invasive techniques to more complex procedures.
Types of Sleep Apnea Surgeries
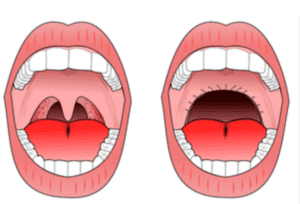
1. Uvulopalatopharyngoplasty (UPPP)
- What It Is: UPPP is one of the most common surgeries for obstructive sleep apnea (OSA). It removes excess tissue from the throat, including parts of the uvula, tonsils, and soft palate, to widen the airway.
- Best for: Mild to moderate OSA patients who have excess throat tissue causing the blockage.
- Effectiveness: Around 50% of patients experience symptom improvement, but it’s less effective for severe OSA.
- Risks: Includes swallowing difficulties, changes in voice, and nasal regurgitation.
2. Genioglossus Advancement (GA)
- What It Is: The Genioglossus Advancement procedure involves moving the tongue muscle attachment forward to prevent the tongue from collapsing into the airway during sleep.
- Best: For patients whose sleep apnea is due to tongue collapse.
- Effectiveness: Generally improves sleep apnea severity by 30-50%.
- Risks: Risks include infection, numbness, and dental issues.
3. Maxillomandibular Advancement (MMA)
- What It Is: MMA is a more invasive procedure that repositions both the upper and lower jawbones to enlarge the airway space.
- Best for: Severe OSA patients who haven’t responded to other treatments.
- Effectiveness: Considered one of the most effective surgical treatments, with success rates up to 90%.
- Risks: Pain, numbness, and long recovery times due to the complexity of the procedure.
4. Hypoglossal Nerve Stimulation (Inspire Therapy)
- What It Is: A small device is implanted under the skin, commonly known as Inspire, which stimulates the hypoglossal nerve, keeping the airway open by controlling tongue movements.
- Best for: Moderate to severe OSA patients who cannot tolerate CPAP and have a certain body mass index (BMI).
- Effectiveness: Studies show a 68-70% reduction in apnea-hypopnea index (AHI) scores.
- Risks: Device malfunction, infection at the implant site, and tingling sensations.
5. Nasal Surgeries
- Types: Includes procedures like septoplasty, turbinate reduction, and nasal polypectomy to improve nasal airflow.
- Best for: Patients with nasal obstructions contributing to OSA.
- Effectiveness: Helps reduce CPAP pressure needs and improve tolerance.
- Risks: Nosebleeds, nasal dryness, or changes in sense of smell.
6. Soft Palate Implants (Pillar Procedure)
- What It Is: This minimally invasive procedure involves placing small implants in the soft palate to stiffen it, reducing airway collapse.
- Best for: Mild to moderate OSA.
- Effectiveness: Provides a 20-30% reduction in AHI scores.
- Risks: Infection, discomfort, and implant extrusion.
Factors to Consider Before Choosing Surgery
1. Severity of Sleep Apnea
- Surgery is typically considered when CPAP therapy fails or for anatomical obstructions causing moderate to severe OSA.
2. Patient’s Age and Health
- Older adults or those with other health complications may not be ideal candidates for surgery due to increased risks during and after the procedure.
3. Previous Treatment History
- If you’ve tried CPAP, oral appliances, or positional therapy without success, surgery might be a logical next step.
4. Anatomical Considerations
- Surgeons often perform imaging tests like cephalometric X-rays or a sleep endoscopy to determine the cause and location of the airway obstruction.
5. Patient Preference and Lifestyle
- Since recovery times and surgical outcomes vary, weighing the potential benefits against the discomfort and downtime associated with surgery is crucial.
Risks and Potential Complications
While sleep apnea surgeries can be effective, they carry certain risks:
- Bleeding and Infection: Common surgical risks that can occur with any procedure.
- Changes in Voice or Swallowing: Particularly relevant for throat surgeries like UPPP.
- Incomplete Symptom Relief: Surgery may not eliminate sleep apnea entirely and may still require CPAP or other therapies post-surgery.
- Long Recovery Times: Particularly with complex procedures like MMA, recovery can take several weeks to months.
What to Expect During Recovery
Recovery experiences vary depending on the procedure:
- Pain Management: Pain is typically managed with medication, and dietary restrictions may be necessary, especially for throat surgeries.
- Follow-Up Sleep Studies: Post-operative sleep studies are often recommended to evaluate the surgery’s success and determine if additional treatments are necessary.
- Lifestyle Adjustments: Temporary modifications like sleeping in an elevated position or using saline sprays for nasal procedures can aid in healing.
Final Thoughts: Is Surgery the Right Choice?
Surgery could possibly be the answer for your sleep apnea. For me, I am happy with my CPAP machine.
I hope you found my article on sleep apnea surgery informative. Of course, you should always consult your doctor first for medical advice.
If you have any comments, please leave them in the comments section below.
Disclaimer: The content on this blog is for informational and educational purposes only and is not a substitute for professional medical advice. Always speak with your doctor or sleep specialist before starting, stopping, or changing any treatment or therapy related to sleep apnea or CPAP use.
Disclaimer: The content on this blog is for informational and educational purposes only and is not a substitute for professional medical advice. Always speak with your doctor or sleep specialist before starting, stopping, or changing any treatment or therapy related to sleep apnea or CPAP use.