Hypercapnia: Understanding the Symptoms and Treatment
As someone who suffers from severe sleep apnea, I try to find out as much as I can about the condition and how it can affect your body.
Today, I’m looking at the condition of Hypercapnia.
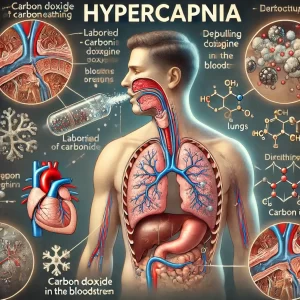
Hypercapnia is a condition characterized by an excess of carbon dioxide (CO2) in the bloodstream.
It often occurs when the lungs are unable to effectively remove carbon dioxide, leading to an imbalance in the body’s gas exchange.
While mild hypercapnia may cause few symptoms, severe cases can be life-threatening and require immediate medical intervention.
In this article, I’ll explore the causes of hypercapnia, its connection to respiratory disorders, symptoms to watch for, and treatment options.
What Is Hypercapnia?
Hypercapnia occurs when there is too much carbon dioxide in the blood, leading to an increase in blood acidity (respiratory acidosis).
Normally, carbon dioxide is expelled through breathing, but when the respiratory system is compromised, the body can’t eliminate CO2 effectively, causing it to accumulate.
This condition is often linked to hypoventilation, which occurs when a person breathes too slowly or shallowly, reducing the amount of CO2 exhaled. As CO2 levels rise, the body becomes unable to maintain the proper balance between oxygen and carbon dioxide, which can lead to various symptoms and complications.
Causes of Hypercapnia
There are several potential causes of hypercapnia, most of which are related to respiratory conditions that affect lung function and breathing. Some of the most common causes include:
1. Chronic Obstructive Pulmonary Disease (COPD)
COPD is a progressive lung disease that includes conditions like emphysema and chronic bronchitis. People with COPD often have difficulty exhaling fully, leading to trapped air in the lungs and an inability to expel carbon dioxide. This results in chronic hypercapnia in many patients, especially in the later stages of the disease.
2. Sleep Apnea
Both obstructive sleep apnea (OSA) and central sleep apnea (CSA) can contribute to hypercapnia, particularly if left untreated. In OSA, the airway becomes blocked during sleep, reducing airflow and leading to episodes of hypoventilation. In CSA, the brain fails to send signals to the muscles that control breathing, causing irregular breathing patterns and the build-up of CO2.
3. Obesity Hypoventilation Syndrome (OHS)
People with OHS, also known as Pickwickian syndrome, have difficulty breathing deeply enough to exchange oxygen and carbon dioxide properly.
This condition is common in individuals who are severely overweight and can lead to chronic hypercapnia, especially during sleep.
4. Respiratory Muscle Weakness
Conditions that affect the diaphragm or other muscles involved in breathing, such as amyotrophic lateral sclerosis (ALS) or muscular dystrophy, can result in hypoventilation and the buildup of CO2.
When these muscles weaken, they are unable to properly contract and expand the lungs, making it difficult to exhale carbon dioxide.
5. Sedative Medications
Certain medications, including sedatives and narcotics, can depress the respiratory system, causing slower or shallower breathing.
This can reduce the amount of carbon dioxide that is exhaled, leading to hypercapnia. People taking medications like opioids or benzodiazepines are at higher risk of experiencing this side effect, especially if they already have underlying respiratory conditions.
Symptoms of Hypercapnia
The symptoms of hypercapnia can vary depending on the severity of the condition and how quickly carbon dioxide levels rise. In mild cases, symptoms may be subtle or even go unnoticed. However, as CO2 levels increase, the following symptoms may occur:
- Shortness of breath or difficulty breathing (dyspnea).
- Confusion or cognitive impairment due to insufficient oxygen reaching the brain.
- Headaches, are often described as a dull, throbbing pain.
- Drowsiness or extreme fatigue, which can worsen as CO2 levels rise.
- Flushed skin, particularly in the face, as the blood vessels dilate in response to CO2 buildup.
- Rapid heart rate (tachycardia), as the body attempts to compensate for the lack of oxygen.
- Muscle twitches or tremors due to nervous system dysfunction.
- Dizziness or lightheadedness.
- In severe cases, loss of consciousness or coma can occur if hypercapnia is not treated promptly.
Complications of Hypercapnia
If left untreated, hypercapnia can lead to serious health complications. Chronic hypercapnia can strain the cardiovascular system and increase the risk of conditions like pulmonary hypertension or right-sided heart failure (cor pulmonale).
It can also result in a condition known as hypercapnic respiratory failure, where the body can no longer maintain the necessary oxygen and carbon dioxide balance, leading to life-threatening consequences.
In addition, severe hypercapnia can impair brain function, leading to confusion, lethargy, and, in extreme cases, coma or death.
Diagnosing Hypercapnia
Diagnosing hypercapnia typically involves measuring the levels of carbon dioxide in the blood using an arterial blood gas (ABG) test.
This test assesses the balance between oxygen and carbon dioxide in the blood and provides insight into the body’s gas exchange efficiency. Other diagnostic tests that may be used include:
- Pulse oximetry to measure blood oxygen levels.
- Capnography, which measures exhaled CO2 levels.
- Pulmonary function tests (PFTs) to assess lung capacity and the effectiveness of the lungs in exchanging gases.
- Imaging tests like chest X-rays or CT scans to identify any structural issues in the lungs.
Treatment for Hypercapnia
The treatment for hypercapnia depends on the underlying cause and the severity of the condition. The goal is to improve ventilation and increase the removal of carbon dioxide from the body. Treatment options may include:
1. Non-Invasive Ventilation (NIV)
For people with conditions like COPD or sleep apnea, non-invasive ventilation (NIV) therapies, such as CPAP (Continuous Positive Airway Pressure) or BiPAP (Bilevel Positive Airway Pressure), can help improve breathing and prevent CO2 buildup.
These machines deliver pressurized air to keep the airway open and support proper ventilation during sleep.
2. Oxygen Therapy
In some cases, oxygen therapy may be used to increase oxygen levels in the blood. However, care must be taken when administering oxygen to patients with COPD, as it can sometimes worsen hypercapnia by reducing the drive to breathe. The goal is to find the right balance between oxygen delivery and CO2 removal.
3. Medications
Certain medications may be prescribed to treat the underlying condition causing hypercapnia. For example, bronchodilators or steroids can help open the airways in people with COPD, improving airflow and gas exchange.
For patients with respiratory muscle weakness, medications to support muscle function may also be used.
4. Lifestyle Changes
For people with obesity hypoventilation syndrome or sleep apnea, weight loss can improve lung function and reduce the risk of hypercapnia. In addition, making lifestyle changes such as quitting smoking and avoiding sedative medications can reduce the likelihood of experiencing CO2 buildup.
5. Mechanical Ventilation
In severe cases of hypercapnic respiratory failure, mechanical ventilation may be required. This involves using a machine to assist or take over the breathing process, ensuring that carbon dioxide is properly exhaled and oxygen is delivered to the body.
Conclusion: Managing Hypercapnia
Hypercapnia can be a serious condition, especially when left untreated. However, with early diagnosis and proper management, the symptoms of hypercapnia can be controlled, allowing individuals to live healthier, more comfortable lives.
If you experience symptoms of hypercapnia, such as shortness of breath or confusion, it’s important to seek medical attention. By addressing the underlying cause and following an appropriate treatment plan, you can reduce the risk of complications and improve your respiratory health.
Thanks for reading my article on Hypercapnia. As always, please seek medical advice if you are concerned about your health.