A Comprehensive Guide of UPPP for Sleep Apnea
What Is Uvulopalatopharyngoplasty?
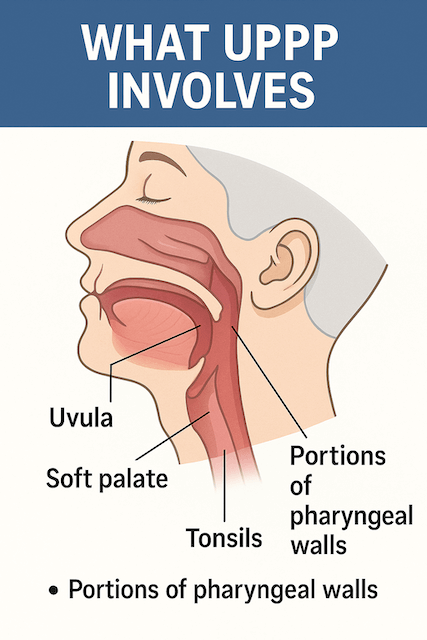
Uvulopalatopharyngoplasty — usually shortened to UPPP — is one of the most common surgical treatments for obstructive sleep apnea (OSA). It involves removing or reshaping tissue from the back of the throat, including parts of the uvula, soft palate, and sometimes the tonsils or pharyngeal walls.
The goal is simple: widen the airway so it collapses less during sleep, reducing the number of apnea events.
This surgery has been around for decades, and while it’s not as commonly performed today (thanks to CPAP therapy and newer options like the Inspire implant), it still plays an important role for certain patients.
A Short History of UPPP
UPPP was first introduced in the early 1980s as doctors searched for surgical solutions to OSA. At the time, CPAP machines were bulky and not widely accepted, so surgery looked like a promising alternative.
Over the years, however, long-term studies showed that UPPP had mixed success rates. Many patients improved, but others continued to experience apneas or even relapsed over time.
Today, UPPP is usually reserved for:
- People who cannot tolerate CPAP therapy
- Patients with specific anatomical features (like an elongated uvula or large tonsils)
- Cases where other less invasive treatments haven’t worked
How the Surgery Works
During UPPP, an ENT surgeon removes or reshapes tissue at the back of your throat. This may include:
- Part of the uvula (the soft tissue that hangs at the back of your throat)
- A section of the soft palate
- Tonsils and adenoids if they’re still present
- Portions of the pharyngeal walls if needed
The procedure is usually performed under general anesthesia and takes about 60–90 minutes. Most people go home the same day or after one night in the hospital.
Recovery After UPPP
Recovery is often described as painful but manageable. For about 1–2 weeks, you can expect:
- Significant throat pain (similar to or worse than a tonsillectomy)
- Difficulty swallowing solid foods
- Temporary changes in speech or swallowing reflex
- Risk of bleeding or infection
Most people return to work in 2–3 weeks, though complete healing can take longer.
Personal note: I’ve never had UPPP myself, but people I’ve spoken to in support groups often describe the recovery as “brutal.” On the flip side, many also say they’d do it again if it meant fewer apneas.
How Effective Is UPPP?
Effectiveness depends heavily on the individual. Studies suggest:
- Success rates range from 40% to 60% when “success” means cutting apnea events in half.
- People with mild to moderate OSA generally see better results than those with severe OSA.
- Success is more likely when enlarged tonsils or a long uvula are contributing to obstruction.
The catch? Even if UPPP improves symptoms, it rarely eliminates OSA entirely. Many patients still need CPAP, an oral appliance, or additional surgery.
Risks and Side Effects
Like all surgeries, UPPP comes with risks. The most common ones include:
- Painful recovery (especially swallowing)
- Voice changes — some patients notice a permanent shift in tone or resonance
- Difficulty swallowing (dysphagia), especially for liquids
- Nasal regurgitation (liquids entering the nose during swallowing)
- Persistent or recurrent sleep apnea — symptoms may return within a few years
In rare cases, scarring from surgery can make CPAP therapy harder to tolerate if it’s needed later.
UPPP vs Other Sleep Apnea Treatments
It’s important to see UPPP as one option among many. Here’s how it compares to other treatments:
CPAP Therapy
- Gold standard for OSA
- Highly effective when used consistently
- Non-surgical and reversible
- Downsides: discomfort, air leaks, and compliance issues
👉 If you’re new to CPAP, my Beginner’s Guide to Sleep Apnea explains how to get started.
Inspire Therapy (Hypoglossal Nerve Stimulation)
- A surgically implanted device that stimulates tongue muscles to keep the airway open
- Often considered after CPAP failure
- High success rates for moderate-to-severe OSA
- Downsides: expensive, requires surgery, not suitable for everyone
👉 See my Sleep Apnea Surgery Guide for a full Inspire overview.
Oral Appliance Therapy
- Custom-made dental devices that reposition the jaw or tongue
- Best for mild to moderate OSA
- Portable and non-invasive
- Downsides: less effective for severe OSA, may cause jaw discomfort
Who Is a Good Candidate for UPPP?
UPPP is usually considered if:
- You’ve tried CPAP and cannot tolerate it
- You have anatomical issues like large tonsils or elongated palate
- Your OSA is mild to moderate
- You’re willing to accept the risks and recovery time
It’s less effective for people with severe obesity or very severe OSA, where CPAP remains the first-line treatment.
Insurance and Cost Considerations
In the U.S., most insurance companies (including Medicare) cover UPPP if it’s deemed medically necessary. This usually requires:
- A sleep study confirming OSA
- Documentation that CPAP was tried and not tolerated
- Recommendation from an ENT or sleep specialist
Out-of-pocket costs can vary widely but typically range from $3,000 to $10,000 before insurance.
Preparing for UPPP Surgery
If you and your doctor decide UPPP is right for you, here are some practical steps:
- Ask questions: What exactly will be removed? What’s the expected success rate in your case?
- Plan your diet: Stock up on soft foods like smoothies, yogurt, and soups.
- Arrange time off work: Expect at least 2 weeks of downtime.
- Line up support: You’ll need someone to drive you home and help during the first few days.
- Stop smoking and limit alcohol: Both slow healing and worsen OSA.
Lifestyle Factors After Surgery
Even if UPPP helps, lifestyle changes still matter. Losing weight, avoiding alcohol before bed, and sticking to a consistent sleep schedule all reduce apnea severity. Some people find that combining UPPP with ongoing CPAP therapy or positional therapy gives the best results.
Frequently Asked Questions
Q: Does UPPP cure sleep apnea?
Not always. UPPP may reduce apneas but often doesn’t eliminate them completely. Many patients still need additional treatment.
Q: How long does UPPP last?
Some patients enjoy lasting relief, while others see symptoms return after a few years. Regular follow-ups are essential.
Q: Is UPPP more effective than Inspire therapy?
For many patients, Inspire has higher long-term success rates. But UPPP may be more appropriate if your anatomy is the main issue or if Inspire isn’t covered by insurance.
Q: Is the recovery really painful?
Yes — most people report significant throat pain for 1–2 weeks. Good pain management and a soft food diet are key.
Q: Can I still use CPAP after UPPP?
Yes, but scarring can make mask fitting or airway pressure less comfortable. Work with your doctor to adjust settings if needed.
Final Thoughts
Uvulopalatopharyngoplasty (UPPP) isn’t the right choice for everyone, but for some patients, it can reduce apnea events and improve quality of life. If you’ve struggled with CPAP or have anatomical issues contributing to OSA, it’s worth discussing with an ENT or sleep specialist.
Just remember: UPPP is not a guaranteed cure. It works best as part of a comprehensive treatment plan that may still include CPAP, oral appliances, or lifestyle changes.
When I was diagnosed with severe OSA in 2014, CPAP became my lifeline. I’ve stuck with it and had great success. But I know people in my support groups who chose UPPP and found real relief — others, not so much. The key is making an informed choice with your doctor, weighing the risks and benefits.
👉 Want to compare more options? Check out my full guide on Sleep Apnea Surgery.
⚠️ MEDICAL DISCLAIMER This blog provides general information only and is not a substitute for professional medical advice, diagnosis, or treatment. Sleep apnea is a serious condition, and CPAP equipment should be used under proper medical supervision. Always consult your doctor or sleep specialist before starting, stopping, or changing any therapy. I share personal experiences as a CPAP user, not as a medical professional. Individual results vary. For medical guidance, please consult a qualified clinician or the American Academy of Sleep Medicine (aasm.org).