Can Sleep Apnea Cause Seizures: Is there a link?
When I was first diagnosed with severe sleep apnea, I assumed my symptoms began and ended with snoring and grogginess. But over time, I learned something deeper — untreated apnea doesn’t just make you tired; it changes the way your brain behaves.
I still remember mornings when I’d wake up light-headed and foggy, unable to focus for hours. That lack of oxygen overnight felt like running on half power all day. And for people who live with epilepsy or seizure disorders, that same oxygen instability can become a serious trigger.
So, can sleep apnea cause seizures? Not directly — but it can create the perfect conditions for them. Let’s break down the science, symptoms, and solutions in a way that actually makes sense.
What Are Sleep Apnea and Seizures?
What Is Sleep Apnea?
Sleep apnea is a sleep disorder where breathing repeatedly stops and starts during sleep. These pauses (called apneas) last anywhere from a few seconds to over a minute.
There are two main forms:
- Obstructive Sleep Apnea (OSA): Throat muscles relax, blocking airflow.
- Central Sleep Apnea (CSA): The brain fails to send breathing signals.
Both lead to oxygen dips (hypoxia) and prevent the brain from entering deep, restorative sleep cycles.
💡 Learn the full difference in What Is Sleep Apnea?
What Are Seizures?
A seizure is a sudden burst of abnormal electrical activity in the brain. It can cause muscle jerks, confusion, or full-body convulsions.
While epilepsy is the most well-known cause, other factors — including sleep deprivation and oxygen loss — can trigger seizures in people without epilepsy too.
💡 Related: Sleep Apnea and Brain Fog
How Sleep Apnea Affects the Brain
During healthy sleep, the brain cycles through light, deep, and REM stages — each responsible for memory, healing, and hormonal balance. When apnea breaks those cycles, the brain never fully resets.
The Oxygen Connection
Each apnea event deprives the brain of oxygen. When oxygen levels drop repeatedly, neurons become overstimulated, increasing the likelihood of electrical misfires. For someone already predisposed to seizures, that’s like throwing sparks onto dry tinder.
Think of your brain as a phone battery that’s constantly unplugged before it reaches 100%. It works, but it’s always unstable.
Neurochemistry in Chaos
Apnea also disrupts neurotransmitters like GABA (which calms brain activity) and glutamate (which excites it). When these get out of sync, your brain stays “wired” even during rest — making seizures more likely.
Studies suggest that long-term oxygen instability changes how the brain handles sleep-stage transitions — especially REM, the phase most vulnerable to apnea events.
💡 For more on the biology of sleep, visit What Is Sleep?
Recognizing the Signs and Getting Diagnosed
Common Clues of Sleep Apnea
- Loud snoring or gasping sounds during sleep
- Unrefreshing sleep despite full nights in bed
- Morning headaches or dry mouth
- Sudden nighttime awakenings
- Daytime sleepiness or brain fog
For people with epilepsy, these symptoms can go unnoticed because they’re overshadowed by seizure management. But ignoring apnea can make seizures harder to control.
Diagnosis
A sleep study (polysomnography) monitors breathing, brain waves, and oxygen saturation. You can even take an At-Home Sleep Apnea Test if you suspect mild apnea.
Your results show whether breathing disruptions are caused by blocked airways (OSA) or misfired brain signals (CSA). Either way, the fix begins with oxygen stability.
What the Science and Data Reveal
Up to 50% of people with epilepsy also have some form of sleep-disordered breathing. The two conditions fuel each other: apnea fragments sleep, and seizures further disrupt recovery.
What Research Shows
- A 2021 study in Epilepsy & Behavior found that patients who began CPAP therapy experienced fewer seizures and improved cognition.
- Another review found that nearly one-third of epileptic patients with untreated apnea saw seizure improvement once their sleep stabilized.
Case Example
A 48-year-old man with long-term epilepsy saw his nocturnal seizures worsen. A sleep study revealed moderate OSA. After six weeks of consistent CPAP therapy, his monthly seizures dropped from five to one. His neurologist reduced his medication for the first time in years.
💡 See how apnea affects the body in Sleep Apnea and Cardiovascular Health
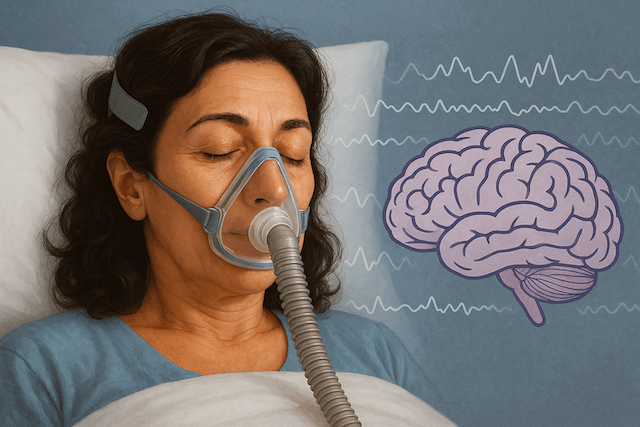
How CPAP Therapy Helps Prevent Seizures
I’ve been using CPAP for over a decade. When I first started, I didn’t realize how much it would change my mental clarity. Within weeks, I could remember names, focus longer, and even felt emotionally steadier.
That’s because CPAP does more than restore breathing — it gives your brain a consistent supply of oxygen.
Why CPAP Works
- Keeps airways open → steady oxygen levels
- Prevents micro-awakenings → allows full REM cycles
- Reduces neural stress → stabilizes brain activity
| Effect | Without CPAP | With CPAP |
|---|---|---|
| Oxygen levels | Fluctuating | Stable all night |
| Seizure frequency | Higher | Up to 50% fewer |
| Sleep quality | Fragmented | Restorative |
| Cognition | Impaired | Sharper, calmer focus |
💡 Compare options in Best CPAP Machines and learn to Stay Consistent with CPAP Therapy
Lifestyle and Prevention: Supporting the Brain Naturally
Treating sleep apnea is step one — but lifestyle changes make it more effective.
Smart Habits for Better Sleep and Fewer Seizures
- Maintain a regular sleep schedule: The brain loves rhythm.
- Sleep on your side: It reduces airway collapse.
- Avoid alcohol and sedatives: They relax throat muscles.
- Manage weight: Extra tissue around the neck increases apnea risk.
- Practice relaxation before bed: Deep breathing or meditation can lower seizure threshold stress.
💡 Read more in Reverse Sleep Apnea Naturally
Taking Charge of Your Sleep Health
If you live with epilepsy, apnea, or unexplained nighttime events — take control with this plan:
- Schedule a sleep study. Even mild apnea affects seizure control.
- Track your nights. Note choking, jerks, or awakenings.
- Use your CPAP every night. Consistency builds neurological stability.
- Collaborate with your doctors. Neurologist + sleep specialist = best outcomes.
- Upgrade your gear. A comfortable mask prevents frustration.
🩺 Explore Best CPAP Masks for Mouth Breathers
FAQ: Common Questions About Sleep Apnea and Seizures
Can sleep apnea cause seizures in people without epilepsy?
Yes — severe oxygen drops can trigger muscle spasms or “seizure-like” episodes. These are usually hypoxic events, not true epileptic seizures.
Can seizures worsen apnea?
They can. Nocturnal seizures can tighten throat muscles or change breathing rhythm, temporarily mimicking apnea events.
Can CPAP therapy interfere with seizure medications?
No. CPAP is mechanical, not chemical — safe with any medication.
Can sleep apnea trigger nocturnal myoclonus (night jerks)?
Yes. Apnea disrupts deep sleep and can cause sudden muscle twitches as the brain “resets” between oxygen drops.
Will treating sleep apnea improve seizure control?
For most patients, yes. CPAP restores oxygen flow, reduces nighttime brain stress, and lowers seizure frequency.
💡 Learn more about seizure patterns in Sleep Apnea in Children
Conclusion: The Power of Restored Sleep
Sleep apnea doesn’t directly cause seizures — but it fuels the same conditions that make them more likely: low oxygen, restless sleep, and neural overstimulation.
When you treat sleep apnea, you’re not just breathing better — you’re giving your brain the stable environment it needs to function safely.
For anyone living with epilepsy, or simply struggling with sleep quality, a simple sleep study can be life-changing. Don’t wait for another rough night or confusing symptom to take action.
💤 Next: Living with Sleep Apnea and Sleep Apnea and Mental Health
⚠️ MEDICAL DISCLAIMER This blog provides general information only and is not a substitute for professional medical advice, diagnosis, or treatment. Sleep apnea is a serious condition, and CPAP equipment should be used under proper medical supervision. Always consult your doctor or sleep specialist before starting, stopping, or changing any therapy. I share personal experiences as a CPAP user, not as a medical professional. Individual results vary. For medical guidance, please consult a qualified clinician or the American Academy of Sleep Medicine (aasm.org).