Central Sleep Apnea: Causes, Symptoms, and Solutions
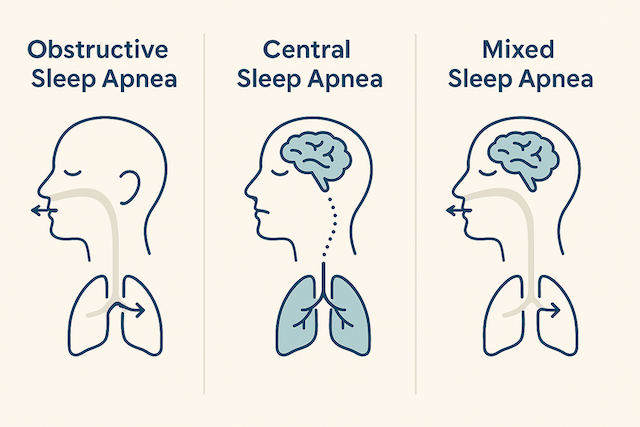
When I was diagnosed with obstructive sleep apnea (OSA), I thought I understood how sleep apnea worked — the airway collapses, oxygen drops, and CPAP fixes the problem.
However, over the years, as I delved into sleep medicine research and spoke with other patients, I discovered a distinct type of sleep apnea that’s quieter, rarer, and far more enigmatic: central sleep apnea (CSA).
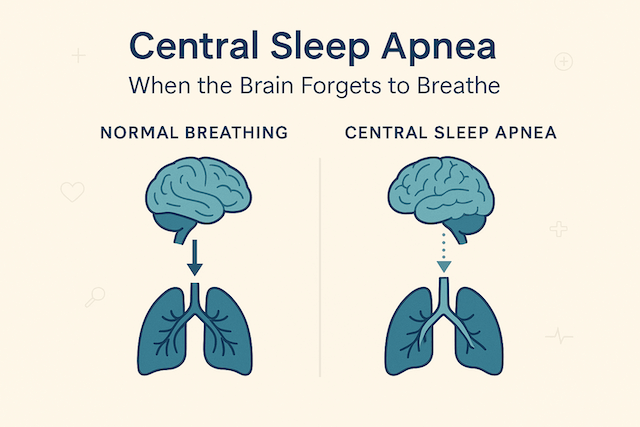
CSA isn’t about an airway collapse. It’s about a missed message.
The brain simply forgets to breathe.
For many people, this discovery comes only after months of frustration: they’ve used CPAP faithfully, their leaks are under control, yet their data still shows “CA events.” If that sounds familiar, this article will walk you through what CSA really is, what the science says, and what real patients have experienced.
What Exactly Is Central Sleep Apnea?
In central sleep apnea, breathing stops for at least 10 seconds — not because the throat is blocked, but because the brain fails to send the signal to breathe. The airway is open, but there’s no effort.
The American Academy of Sleep Medicine defines it as “a cessation of airflow and respiratory effort for ≥10 seconds due to absent ventilatory drive.” In plain English: your lungs are ready, but the command never comes.
CSA affects roughly 1% of adults over 40, though it’s far more common in those with heart failure, neurological disorders, or those taking opioids that suppress the brain’s respiratory centers. (Sleep Foundation)
Unlike obstructive apnea, which is mechanical, CSA is neurological — a control system problem rather than a plumbing one.
The Science Behind CSA
During sleep, your breathing is controlled automatically by your brainstem, based on the level of carbon dioxide (CO₂) in your blood. When CO₂ rises, the brain triggers you to inhale. When CO₂ drops too low, breathing pauses until it builds back up again.
In people with CSA, that balance is unstable. Their brain overshoots — they breathe too deeply, CO₂ drops sharply, and then their brain “forgets” to restart breathing until levels climb again. This creates a rhythm of over-breathing followed by silence.
One of the best descriptions I’ve read comes from a 2024 Frontiers in Sleep case study:
“In patients with unstable ventilatory control, central apneas emerge as the feedback loop oscillates between hyperventilation and apnea.”
It’s not a blockage — it’s a miscalibration.
Real People, Real Cases
I can talk theory all day, but nothing brings clarity like real-world stories. Here are three published cases that reveal how diverse CSA can be.
1. The Woman Whose Medication Triggered CSA
A 60-year-old woman began low-dose baclofen for muscle spasms — just 10 mg twice daily. Within weeks, she developed nighttime choking and severe fatigue. Her sleep study showed repeated central apneas. When her physician stopped the baclofen, her breathing returned to normal.
The case, published in Journal of Medical Case Reports (2025), illustrates how medications that act on the brain’s GABA system can suppress the drive to breathe.
Takeaway: Always review your medication list if new central events appear on therapy. Even small doses can matter.
2. The Patient Whose “Treatment-Emergent” CSA Hid a Brain Tumor
Another story comes from CHEST Journal (2024). A woman diagnosed with OSA began CPAP therapy, but her machine data showed persistent central events. Even after switching to ASV, her fatigue worsened. Imaging later revealed a meningioma compressing her brainstem. After surgical removal, her sleep apnea resolved.
Takeaway: Not every central event is benign. If your central apnea index rises or symptoms worsen despite proper therapy, ask about a neurologic workup — especially if accompanied by headaches, imbalance, or new neurologic symptoms.
3. The Heart-Failure Patient Whose CSA Disappeared
A 69-year-old man with severe heart failure suffered from both obstructive and central apneas, including Cheyne–Stokes respiration — a distinctive pattern of waxing and waning breathing. After implantation of a left ventricular assist device (LVAD), his oxygen levels normalized, and both OSA and CSA disappeared entirely.
That story, published in Frontiers in Sleep, shows how CSA isn’t always the disease itself — sometimes it’s a symptom of another system out of rhythm.
Takeaway: If CSA appears alongside heart failure, optimizing cardiac function can sometimes “cure” the sleep apnea.
Cheyne–Stokes Respiration
A cyclical breathing pattern where airflow gradually increases and decreases in a wave-like rhythm. It’s commonly linked with heart failure and stroke.
Read my full breakdown of Cheyne–Stokes respiration and how it affects heart health and sleep.
Recognizing the Signs
Because CSA doesn’t cause the same snoring or gasping as OSA, it often goes unnoticed.
Common symptoms include:
- Persistent fatigue, even after months of CPAP use
- Morning headaches
- Waking short of breath or with a racing heart
- Fragmented sleep without clear airway obstruction
- Data showing “CA events” on a CPAP report
If your machine shows consistent central apneas, don’t ignore it. Bring it to your provider’s attention — you may need a follow-up polysomnography (sleep study) to confirm whether those events are truly central.
Diagnosing CSA
A sleep study distinguishes central from obstructive events by looking for chest and abdominal effort.
- In OSA, your chest moves — you’re trying to breathe but can’t.
- In CSA, there’s no effort. The signal simply isn’t sent.
Modern sleep labs also measure CO₂ levels, heart rhythm, and oxygen desaturation to confirm the pattern and its cause.
In persistent or unexplained cases, imaging (MRI or CT) can identify neurological factors, as seen in the meningioma patient above.
In some rare cases, central sleep apnea can stem from structural issues in the brain or brainstem — for example, Chiari malformations, where tissue at the base of the skull presses on areas that control breathing. If your doctor suspects a neurological cause, imaging such as MRI is often recommended.
Learn more about Chiari malformations and their role in sleep-disordered breathing
Treatment Options (and What Science Says Works)
There’s no single fix for CSA because it’s not a single condition.
Here’s what current research — and my own conversations with clinicians — show.
CPAP with Backup Rate
For mild CSA or treatment-emergent CSA, a CPAP device that provides a timed backup breath can stabilize breathing. Studies show roughly 50% of such patients improve with standard CPAP alone (Springer Sleep & Breathing, 2024).
Adaptive Servo-Ventilation (ASV)
ASV continuously monitors each breath and adjusts pressure in real time. It’s widely regarded as the gold standard for moderate-to-severe CSA — especially Cheyne–Stokes respiration.
However, it’s contraindicated for some heart-failure patients with reduced ejection fraction (per the SERVE-HF trial).
BiPAP-ST
This “spontaneous/timed” mode helps patients whose brains generate inconsistent breathing effort. It provides mandatory breaths when natural ones don’t occur.
Supplemental Oxygen
For altitude-related or mild CSA, supplemental oxygen can reduce events by stabilizing oxygen saturation.
Treating the Underlying Cause
When CSA stems from heart failure, opioids, or neurological disease, treating that root issue can reduce or eliminate apnea events.
Emerging research also suggests that phrenic nerve stimulation may be a potential therapeutic option. Early studies suggest promising results, but long-term data are still limited (MDPI Journal of Clinical Medicine, 2024).
Living with CSA
Even though I don’t personally have central sleep apnea, I’ve spoken to dozens of people who do.
They describe it less as a breathing problem and more as a confidence problem — the feeling that your body can’t be trusted to keep breathing when you sleep.
What helps most, in their words, is knowledge and collaboration.
Here’s what they’ve shared — and what I’ve learned as a fellow CPAP user:
- Track your data weekly. Don’t obsess daily — look for trends, not nights.
- Ask better questions: “Are my central events resolving?” “Should I consider ASV?” “Could my medications play a role?”
- Revisit your heart health: many patients discover their CSA improves as cardiac therapy stabilizes.
- Stay consistent: therapy adjustments take time — weeks, not nights.
What the Evidence Shows About Outcomes
CSA carries more than sleep consequences — it can influence heart rhythm, blood pressure, and even mortality risk.
A 2024 Sleep and Breathing meta-analysis found that untreated CSA in heart-failure patients correlated with a 30–40% increase in cardiac events.
But that’s not the whole story. Patients who received optimized therapy (ASV or cardiac management) often saw significant improvement — sometimes full resolution.
That aligns with what I’ve seen: the sooner you identify the cause, the better the recovery trajectory.
Final Thoughts
If OSA is about obstruction, CSA is about communication — the delicate conversation between your brain and your lungs.
For some, it’s temporary. For others, it’s chronic.
But in nearly every case, it’s manageable with the right evaluation and therapy.
If your data shows central events, don’t dismiss them — but don’t panic either. Bring your sleep physician the full picture: data, symptoms, and medications. The right combination of science, persistence, and partnership can turn confusion into clarity — and sleeplessness into stability.
⚠️ MEDICAL DISCLAIMER This blog provides general information only and is not a substitute for professional medical advice, diagnosis, or treatment. Sleep apnea is a serious condition, and CPAP equipment should be used under proper medical supervision. Always consult your doctor or sleep specialist before starting, stopping, or changing any therapy. I share personal experiences as a CPAP user, not as a medical professional. Individual results vary. For medical guidance, please consult a qualified clinician or the American Academy of Sleep Medicine (aasm.org).