Pickwickian Syndrome
Pickwickian Syndrome, medically known as Obesity Hypoventilation Syndrome (OHS), is a serious condition that often goes hand-in-hand with sleep apnea, particularly obstructive sleep apnea (OSA). Characterized by a combination of obesity and inadequate breathing, especially during sleep, Pickwickian Syndrome can lead to a host of health complications if left untreated.
In this article, we’ll explain Pickwickian Syndrome, how it’s diagnosed, its symptoms, and what treatment options are available to help manage the condition.
What Is Pickwickian Syndrome?

Pickwickian Syndrome was named after the character Joe from Charles Dickens’s novel The Pickwick Papers, who exhibited symptoms like extreme obesity and sleepiness. The medical condition, however, involves a more specific set of problems related to breathing and oxygen levels.
At its core, Pickwickian Syndrome refers to obesity hypoventilation, which occurs when someone with a high body mass index (BMI) has trouble breathing deeply or effectively. This results in high levels of carbon dioxide (CO2) in the blood and lower levels of oxygen, particularly during sleep.
While obstructive sleep apnea causes temporary airway blockages during sleep, Pickwickian Syndrome is characterized by chronic under-breathing, both day and night. The two conditions often occur together, worsening each other’s effects and making diagnosis and treatment more complex.
What are the Symptoms
The symptoms of Pickwickian Syndrome often overlap with those of sleep apnea, but they also include signs of the body’s inability to properly regulate oxygen and carbon dioxide levels.
Common symptoms include:
- Excessive daytime sleepiness: A hallmark of Pickwickian Syndrome, people often feel drowsy during the day, regardless of their sleep.
- Shortness of breath: Difficulty breathing during physical activity or even while resting is common in people with this syndrome.
- Loud snoring: Most individuals with Pickwickian Syndrome also have sleep apnea, which causes loud snoring and interruptions in breathing.
- Morning headaches: These headaches are caused by elevated CO2 levels during the night due to inadequate breathing.
- Fatigue: Frequent complaints are chronic tiredness, mental fog, and decreased energy.
- Cyanosis (bluish skin): Low oxygen levels may lead to blue-tinged lips or skin.
- Swelling of the legs or ankles: This symptom can indicate heart strain, which is often exacerbated by oxygen deficiency and fluid retention.
Personal Insight: Before being diagnosed with severe obstructive sleep apnea, I didn’t realize how much my weight could affect my sleep apnea, not just at night but even during the day. That is why I embarked on an exercise program.
Causes and Risk Factors
The exact cause of Obesity Hypoventilation Syndrome (OHS), which medical professionals like to refer to this condition as isn’t fully understood, but it’s widely accepted that the condition arises from the combination of obesity and impaired breathing regulation. Obesity puts pressure on the chest wall and diaphragm, which makes it harder for the lungs to expand fully. This shallow breathing leads to carbon dioxide retention and a decrease in oxygen levels.
Risk factors for developing Pickwickian Syndrome include:
- Obesity: A BMI over 30 is a key risk factor, and the risk increases with higher BMI levels.
- Obstructive Sleep Apnea (OSA): Many people with Pickwickian Syndrome also have OSA, which further complicates breathing patterns.
- Age: While Pickwickian Syndrome can develop in younger individuals, it is more commonly diagnosed in middle-aged adults.
- Gender: Men are more likely to develop OHS, although the condition also affects women, particularly post-menopause.
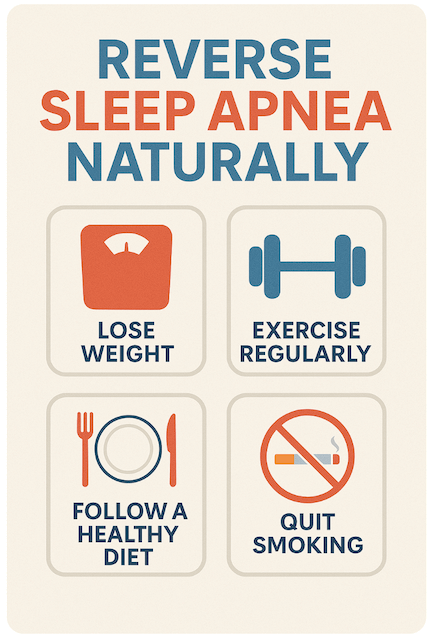
- Sedentary Lifestyle: Lack of regular physical activity can exacerbate weight gain and breathing issues.
Personal Insight: I was always aware of how my weight affected my daily life, but I didn’t understand that it was also causing my breathing to slow down, even when I wasn’t asleep. My sleep doctor explained that my body wasn’t getting enough oxygen at night, which contributed to my exhaustion and breathlessness during the day.
Diagnosing OHS
Diagnosing this syndrome typically requires a combination of tests to measure breathing function, oxygen levels, and carbon dioxide retention. Since the symptoms often overlap with sleep apnea, a full diagnostic evaluation is essential to distinguish between the two conditions or confirm if both are present.
Some common tests include:
- Arterial Blood Gas (ABG) Test: This test measures the levels of oxygen and carbon dioxide in your blood to determine whether hypoventilation (underbreathing) is occurring.
- Pulmonary Function Tests: These tests measure how well your lungs are working by assessing how much air you can inhale and exhale.
- Sleep Study (Polysomnography): If sleep apnea is suspected, a sleep study may be recommended to monitor breathing patterns during sleep, detect pauses in breathing, and measure oxygen levels.
- Overnight Oximetry: This test measures blood oxygen levels during sleep, helping detect oxygen desaturation at night.
A diagnosis of Pickwickian Syndrome is confirmed when the following are present:
- Obesity (BMI > 30)
- Hypoventilation (elevated CO2 levels)
- No other significant cause of hypoventilation, such as lung or neuromuscular disease
Personal Insight: When I went for my sleep study, the results not only showed severe sleep apnea but also low oxygen levels that continued even when I was awake. It was a relief to finally understand what was causing my constant fatigue and shortness of breath, but it also made me realize how serious untreated sleep disorders could be.
Treatment Options for OHS
Treating Pickwickian Syndrome usually involves a combination of lifestyle changes and medical interventions. The primary goals of treatment are to improve breathing, reduce carbon dioxide retention, and restore normal oxygen levels.
1. Weight Loss
- Diet and Exercise: Weight loss is often the first recommendation, as reducing body weight can significantly improve breathing patterns and oxygen levels. Even a modest weight loss can help alleviate symptoms of both OHS and sleep apnea.
- Bariatric Surgery: For those who struggle to lose weight through diet and exercise alone, bariatric surgery may be recommended as a way to promote significant and sustained weight loss.
2. CPAP or BiPAP Therapy
- Many people with Pickwickian Syndrome also suffer from sleep apnea, which makes CPAP (Continuous Positive Airway Pressure) therapy a crucial part of treatment. CPAP helps keep the airway open during sleep, ensuring continuous oxygen flow and preventing apneas.
- BiPAP (Bilevel Positive Airway Pressure) may be used in more severe cases. BiPAP delivers different pressure levels for inhalation and exhalation, making breathing easier, especially for those with hypoventilation issues.
3. Oxygen Therapy
- In some cases, supplemental oxygen may be needed, particularly if oxygen levels are severely low. This therapy can be delivered through nasal prongs or a mask to ensure adequate oxygen is available during both waking and sleeping hours.
4. Medication
- Medications that stimulate breathing, such as acetazolamide or theophylline, may sometimes be prescribed, though they are less common. These drugs can help increase respiratory drive and reduce CO2 levels in the blood.
5. Regular Monitoring
- People with Pickwickian Syndrome require ongoing medical monitoring to assess treatment effectiveness and adjust therapies as needed. This might include follow-up sleep studies, regular blood gas tests, and pulmonary function tests.
Personal Insight: After being diagnosed with sleep apnea, starting CPAP therapy changed my life. I can only imagine how much more difficult it would have been to manage if I had also been dealing with OHS. From what I’ve learned, getting the right treatment—whether it’s CPAP or BiPAP—can make a huge difference in how well you sleep and feel throughout the day.
Conclusion
OHS is a complex condition that often coexists with sleep apnea. If left untreated, it can significantly impact one’s quality of life. However, with proper diagnosis and treatment, many people can manage the condition effectively. Weight loss, CPAP or BiPAP therapy, and regular medical monitoring can help restore normal breathing and improve overall health.
If you suspect you might have Pickwickian Syndrome, consult with a healthcare provider to explore your options. Early intervention can lead to better outcomes and, in many cases, a significant improvement in your symptoms and daily energy levels.
Personal Insight: Learning about the connection between weight and breathing issues was a big eye-opener for me. While I don’t have Pickwickian Syndrome, I now understand how untreated sleep apnea can lead to more severe health problems like OHS.
If you’re struggling with breathing issues and weight, don’t hesitate to seek medical advice—it could be the key to a healthier and more energized life.