Sleep Apnea Diagnosis – Understanding the Condition
Jeremy Smith is a long-term CPAP user and sleep apnea advocate. After being diagnosed with severe obstructive sleep apnea, he created ByJeremySmith.com to help others navigate CPAP therapy through personal stories, gear reviews, and practical advice.
Sleep apnea is a severe sleep disorder that affects millions of people worldwide, and getting a proper sleep apnea diagnosis is crucial.
I am one of these people.
It often goes undiagnosed for years, leaving those affected to struggle with poor sleep, fatigue, and increased health risks.
This picture represents me. I was happy when I received my sleep apnea diagnosis because it answered all the questions I had about my headaches and migraines.
Getting a proper sleep apnea diagnosis is essential for improving sleep quality and overall well-being. In this article, I will dive into the symptoms, causes, risk factors, diagnostic process, and treatments for sleep apnea, offering a comprehensive guide to understanding the condition and taking the proper steps for your health.
Getting a formal diagnosis of sleep apnea is something that can dramatically turn your life around. I am speaking from personal experience because, before my diagnosis, I was suffering from daily fogginess as well as migraines that were getting more frequent.
The symptoms may be different for you, so it’s important to get a diagnosis as soon as possible.
How Common is Sleep Apnea?
Sleep apnea is more widespread than many people realize. According to the American Sleep Apnea Association, an estimated 22 million Americans suffer from sleep apnea, with 80% of moderate to severe cases undiagnosed. Globally, the prevalence of obstructive sleep apnea (OSA) is also high, particularly in adults over the age of 40.
- Men are more likely to suffer from sleep apnea than women, though the gap narrows with age and post-menopause.
- The condition is becoming increasingly common due to rising rates of obesity, a significant risk factor for sleep apnea.
- Children and young adults can also be affected, though sleep apnea is often underdiagnosed in these age groups.
It is scary to think of how many people are out there with untreated sleep apnea. These people are not just annoying their partner with loud snoring but potentially shaving years off their lives.
Symptoms of Sleep Apnea
Sleep apnea often presents with various symptoms, many of which may seem unrelated to sleep at first. Here are some of the most common indicators:
- Loud snoring: While not everyone who snores has sleep apnea, loud, chronic snoring is one of the hallmark symptoms, particularly in obstructive sleep apnea (OSA).
- Gasping or choking during sleep: This is a sign that your airway is being blocked or your brain is failing to signal your body to breathe.
- Pauses in breathing: A bed partner may notice that you stop breathing for several seconds at a time, followed by gasps for air.
- Frequent awakenings: These disruptions may not fully wake you up, but they interrupt the sleep cycle, leading to poor-quality sleep.
- Morning headaches: Oxygen deprivation during the night can lead to headaches upon waking.
- Daytime sleepiness: This can manifest as extreme tiredness, even after what seems like a whole night’s sleep.
- Irritability and difficulty concentrating: Poor sleep quality can directly impact your mood and cognitive functions.
These symptoms can lead to serious consequences if untreated, including increased risks of heart disease, high blood pressure, diabetes, and even stroke.
Personal insight: For most of my life, I thought my snoring was just a nuisance to my family, not a health issue. But over time, my fatigue became overwhelming, and I was falling asleep in the middle of the day, dozing during important meetings. It was only after my wife noticed that I stopped breathing during the night that I realized I needed to seek help.
Causes of Sleep Apnea
There are two primary types of sleep apnea, and the causes vary based on which type you have:
- Obstructive Sleep Apnea (OSA): This occurs when the muscles at the back of your throat relax too much, causing the airway to collapse and block airflow. The brain briefly wakes you up to reopen the airway, but this can happen hundreds of times a night without you being aware of it. Common causes include:
- Excess weight or obesity
- Enlarged tonsils or adenoids
- Structural abnormalities in the airway
- Relaxation of muscles due to alcohol or sedatives
- Central Sleep Apnea (CSA): This type of sleep apnea occurs when the brain doesn’t send the proper signals to the muscles that control breathing. CSA is often associated with severe health conditions such as:
- Heart failure
- Stroke
- Neurological disorders like Parkinson’s disease
- Use of certain medications, particularly opioids
- Mixed Sleep Apnea: This is a combination of both obstructive and central sleep apnea, and its causes can include both airway blockages and disrupted brain signals.
Personal insight: In my case, I was diagnosed with obstructive sleep apnea. I did lose 22 pounds but in my case it didn’t help with my sleep apnea.
Risk Factors for Sleep Apnea
Certain factors can increase your risk of developing sleep apnea. While some of these factors are beyond your control, others can be managed or mitigated:
- Obesity: Excess weight, especially around the neck, can put pressure on the airway and increase the likelihood of airway collapse during sleep.
- Age: Sleep apnea becomes more common as you get older, with the highest rates occurring in adults over 40.
- Gender: Men are more likely than women to develop sleep apnea, though post-menopausal women see a significant rise in risk.
- Family history: Sleep apnea can run in families, especially if there’s a genetic predisposition to OSA or certain physical traits like a narrow airway.
- Lifestyle choices: Smoking, alcohol consumption, and the use of sedatives or muscle relaxants can all exacerbate sleep apnea symptoms.
- Medical conditions: Conditions such as heart disease, high blood pressure, diabetes, and even asthma are linked to an increased risk of sleep apnea.
Personal insight: I always thought sleep apnea only affected older men, but after my diagnosis, I realized how many risk factors I had. My weight and even the occasional beer were all contributing to my sleep apnea. Understanding these factors helped me make changes that improved my treatment outcomes.
Diagnosis of Sleep Apnea
If you suspect you have sleep apnea, the first step is to see your healthcare provider.
They may refer you to a sleep specialist who will evaluate your symptoms and recommend a sleep study. The diagnostic process typically includes:
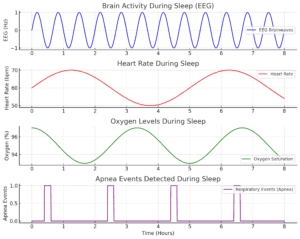
- Polysomnography (PSG): This comprehensive sleep study is conducted in a sleep lab where your brain waves, blood oxygen levels, heart rate, breathing patterns, and body movements are monitored while you sleep.
- Home Sleep Apnea Test (HSAT): For those unable to undergo an in-lab study, a portable device can be used at home to measure oxygen levels, airflow, and breathing effort during sleep. However, this test may not be as accurate for diagnosing central sleep apnea.
- Additional tests: If central sleep apnea is suspected, further tests like an echocardiogram or brain MRI may be needed to identify underlying conditions.
If the sleep study reveals you have sleep apnea, the severity will be measured by what is known as the AHI Apnea-Hypopnea Index. This is basically how many times to stop breathing per minute (an apnea). The more times, the more severe.
Personal insight: Going in for a sleep study was intimidating at first. Sleeping with all those wires attached to me wasn’t exactly appealing, but it gave me the answers I desperately needed.
The results were “eye opening”when I found out I stopped breathing more than 50 times an hour. This is considered sever sleep apnea on the AHI Apnea-Hypopnea Index.
But on the good side, this diagnosis explained a lot of things.
Treatments for Sleep Apnea
The treatment for sleep apnea varies depending on the type and severity of the condition. Some of the most common treatment options include:

- CPAP Therapy (Continuous Positive Airway Pressure): This is the most common treatment for obstructive sleep apnea. A CPAP machine delivers a steady stream of air through a mask to keep the airway open during sleep.
- BiPAP Therapy (Bi-level Positive Airway Pressure): Similar to CPAP but offers two different levels of air pressure for inhalation and exhalation, making it more comfortable for some people with central or complex sleep apnea.
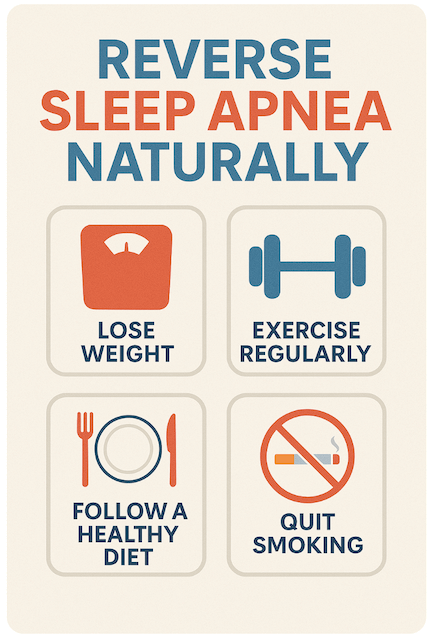
- Lifestyle changes: Weight loss, smoking cessation, and avoiding alcohol or sedatives before bed can significantly improve symptoms.
- Surgery: In severe cases, surgical interventions like Uvulopalatopharyngoplasty (UPPP) or jaw repositioning surgeries may be necessary to remove excess tissue or open the airway.
- Dental devices: Oral appliances designed to keep the throat open can be an alternative for those with mild to moderate OSA.
Personal insight: The CPAP machine took some getting used to, but after a few weeks, I started to notice a dramatic difference in how I felt during the day. I also made some lifestyle changes—like losing weight and avoiding alcohol before bed—which made the treatment even more effective.
Conclusion: Getting the Right Sleep Apnea Diagnosis
A sleep apnea diagnosis can be life-changing in the best way possible. You can improve your sleep and overall health by identifying the condition and getting the proper treatment.
The earlier you seek help, the sooner you can start feeling the benefits of better, uninterrupted sleep.
Personal insight: Looking back, I wish I had sought a diagnosis sooner. Living with untreated sleep apnea affected every part of my life, from my health to my relationships. Now, with the right treatment, I’m finally getting the restful sleep I need—and so is my family!
Do you have any questions regarding Sleep Apnea Diagnosis or any stories? Please share below.
Disclaimer: The content on this blog is for informational and educational purposes only and is not a substitute for professional medical advice. Always speak with your doctor or sleep specialist before starting, stopping, or changing any treatment or therapy related to sleep apnea or CPAP use.