Hypopnea vs Sleep Apnea: Understanding the Key Differences
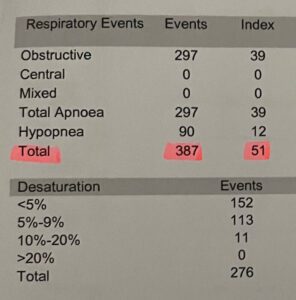
My Wake-Up Call: These are my sleep study results
I’ll never forget the day I received my sleep study results.
It came with mixed feelings…
On one hand, I was relieved that there was something that explained the punding headaches and migraines, but on the other hand, I was thinking about how much damage I had inflicted on my body for so long.
As they say, “You don’t know what you don’t know.”
So I created this blog to give folks an early warning of what might be happening to their bodies.
👉 How to take a Home Sleep Apnea Test
Staring at the numbers on that report felt surreal: 387 total breathing events in a single night. That meant my breathing stopped or significantly slowed down 387 times while I slept. My Apnea-Hypopnea Index (AHI) was 51—placing me firmly in the “severe” category of obstructive sleep apnea.
Breaking it down further, I had experienced 297 complete apneas (where my breathing stopped entirely) with an index of 39 events per hour, and 90 hypopneas (partial breathing restrictions) with an index of 12 per hour. To put that in perspective, I was stopping breathing or taking shallow breaths roughly once every minute throughout the night.
Before that diagnosis, I thought I was just a “bad sleeper.” I’d wake up exhausted no matter how many hours I spent in bed. My wife complained about my thunderous snoring. I’d find myself nodding off during afternoon meetings. Morning headaches were just part of my routine. Sound familiar?
What I didn’t understand then—but learned quickly—was the critical difference between those 297 apneas and those 90 hypopneas. Both were robbing me of oxygen and quality sleep, but in different ways. Understanding this distinction became crucial to understanding my condition and, ultimately, reclaiming my health.
If you’ve been experiencing restless nights, morning headaches, or excessive daytime fatigue, you might have heard terms like “sleep apnea” and “hypopnea” thrown around during medical consultations. While these conditions are closely related and often occur together (as they clearly did in my case), understanding the critical differences between hypopnea vs sleep apnea is essential for proper diagnosis, treatment, and long-term health management.
In this comprehensive guide, we’ll explore everything you need to know about these sleep-disordered breathing conditions, from their fundamental differences to treatment options and long-term health implications.
What Is Sleep Apnea?
Sleep apnea is a common and potentially serious disorder affecting approximately 39 million American adults. During sleep apnea episodes, your airways become fully obstructed, causing you to stop breathing for 10 seconds or more—sometimes up to a minute or longer—during the night.
These complete pauses in breathing can happen dozens or even hundreds of times per night, severely disrupting your sleep quality and causing dangerous drops in blood oxygen levels. Many people don’t even realize they have sleep apnea until a bed partner notices the telltale signs: loud snoring followed by periods of silence, then gasping or choking sounds as breathing resumes.
Types of Sleep Apnea
There are actually three main types of sleep apnea, each with different underlying causes:
Obstructive Sleep Apnea (OSA) is by far the most common form, accounting for about 84% of all sleep apnea cases. OSA occurs when the muscles in the back of your throat relax too much during sleep, causing the soft tissue to collapse and block the airway. This physical obstruction prevents air from flowing into your lungs despite your body’s efforts to breathe.
Central Sleep Apnea (CSA) is less common and works differently. Rather than a physical blockage, CSA happens when your brain fails to send proper signals to the muscles that control breathing. Your body simply “forgets” to breathe for periods during sleep.
Complex Sleep Apnea (also called treatment-emergent central sleep apnea) is a combination of both obstructive and central sleep apnea. This type sometimes develops when someone with OSA begins CPAP therapy.
What Is Hypopnea?
Hypopnea is sleep apnea’s lesser-known but equally troublesome cousin. The term “hypopnea” comes from the Greek words “hypo” (meaning “under” or “below”) and “pnea” (meaning “breathing”). With hypopnea, you take shallow breaths for 10 seconds or longer while asleep, and your airflow is reduced by at least 30% compared to normal breathing levels.
The critical distinction is that breathing doesn’t completely stop since your airway is only partially blocked rather than fully obstructed. However, this partial blockage still significantly reduces oxygen flow to your lungs and can cause many of the same health problems as complete apneas.
Think of it this way: if sleep apnea is like a completely kinked garden hose where no water flows through, hypopnea is like someone stepping partially on the hose—water still flows, just not at full capacity. Both scenarios prevent adequate water (or in this case, oxygen) from reaching its destination.
The Key Difference: Hypopnea vs Sleep Apnea
The fundamental difference between these two conditions lies in the degree of airway obstruction and the resulting impact on breathing:
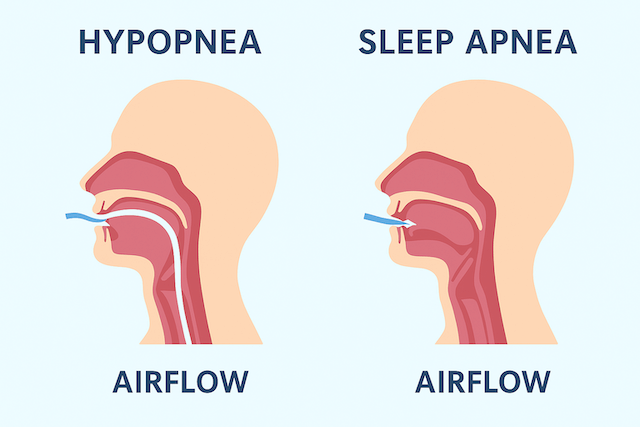
- Sleep Apnea: Complete blockage of the airway causing a 90% or greater reduction in airflow for 10 seconds or more
- Hypopnea: Partial blockage leading to a 30-90% reduction in airflow for 10 seconds or more, rather than total cessation of breathing
While hypopnea is traditionally considered less severe than apnea, recent research has revealed a surprising truth: hypopnea may have a similar—if not indistinguishable—impact on the negative health outcomes associated with sleep-disordered breathing. This means that dismissing hypopnea as “less serious” could be a dangerous mistake.
In clinical practice, many patients experience both apneas and hypopneas throughout the night. In fact, studies have shown that hypopneas occur more frequently than apneas in most patients. One major research study found that patients had a mean hypopnea index of 22.1 events per hour compared to only 4.43 apneas per hour, demonstrating that hypopneas are actually the predominant breathing event for most people with sleep-disordered breathing.
Recognizing the Symptoms
Both conditions share many similar sleep apnea symptoms, making it difficult to distinguish between them without a proper sleep study. Common symptoms include:
Nighttime Symptoms
Before my diagnosis, I didn’t realize how many of these symptoms I was experiencing—I’d normalized them as just “how I sleep.” Looking back, the warning signs were everywhere:
- Loud, chronic snoring that disrupts your partner’s sleep (my wife started sleeping in another room)
- Gasping or choking during sleep
- Witnessed breathing pauses (observed by a bed partner)
- Frequent nighttime awakenings (though you may not remember them)
- Nighttime urination (nocturia)
- Night sweats without other explanation
- Restless sleep with tossing and turning
Daytime Symptoms
- Excessive daytime sleepiness despite spending adequate time in bed
- Morning headaches that typically improve as the day progresses
- Difficulty concentrating or memory problems
- Irritability or mood changes, including depression
- Decreased libido or sexual dysfunction
- Waking with a dry mouth or sore throat
- Brain fog and cognitive difficulties
However, apnea typically produces more dramatic nighttime signs compared to hypopnea. With sleep apnea, you’ll likely experience louder snoring accompanied by complete silence during breathing pauses, followed by more pronounced gasping or choking sounds as your body desperately tries to resume breathing. The distinction can be subtle, which is why professional sleep apnea diagnosis is essential.
Understanding the Apnea-Hypopnea Index (AHI)
Healthcare providers use a crucial measurement called the Apnea-Hypopnea Index (AHI) to diagnose and assess the severity of these conditions. The AHI measures how many times your breathing slows or stops during an average hour of sleep.
How AHI is Calculated
The AHI is calculated using a simple formula:
AHI = (Total number of apneas + Total number of hypopneas) / Total hours of sleep
For example, if you experience 15 apneas and 27 hypopneas over seven hours of sleep, your AHI would be 6 events per hour (42 total events ÷ 7 hours = 6).
AHI Severity Scoring for Adults
Here’s how the scoring works for adults:
- Normal: Fewer than 5 events per hour
- Mild: 5 to 14 events per hour
- Moderate: 15 to 29 events per hour
- Severe: 30 or more events per hour
With my AHI of 51, I was well into the severe category. But here’s what really struck me: my 297 apneas represented an index of 39 events per hour, while my 90 hypopneas had an index of 12 per hour. This showed that while complete breathing stoppages were my primary issue, the partial obstructions were also significant contributors to my overall sleep disruption. Both needed to be addressed for successful treatment.
It’s important to note that children have different AHI criteria. Due to their different physiology, an AHI exceeding 1 is considered abnormal in children, and an AHI of 2 or greater often warrants treatment referral.
Understanding Your Results
Your AHI score is just one piece of the diagnostic puzzle. Healthcare providers also consider:
- Oxygen desaturation levels during breathing events
- Sleep stage distribution (REM vs. non-REM sleep)
- Body position during events
- Frequency of arousals from sleep
- Your symptoms and medical history
Many people who have apnea also experience episodes of hypopnea throughout the night, and vice versa. This is why specialists sometimes combine the two conditions under the term Obstructive Sleep Apnea-Hypopnea (OSAH) or simply refer to the broader category of sleep-disordered breathing.
Who’s at Risk? Understanding Risk Factors
Several factors increase your likelihood of developing hypopnea or sleep apnea. Understanding these risk factors can help you assess your personal risk and take preventive action.
Lifestyle and Behavioral Factors
Excess Weight and Obesity: This is the leading risk factor for obstructive sleep apnea. Extra pounds can build up fat deposits in your neck and around the airway, physically narrowing the passage and making obstruction more likely. The good news? CPAP therapy and weight loss work synergistically—treating sleep apnea can actually help with weight loss efforts.
Smoking: Smoking irritates and inflames airway tissues, increasing fluid retention and swelling in the upper airway by three times compared to non-smokers. Secondhand smoke also increases risk.
Alcohol and Sedatives: Consuming alcohol or taking sedatives before bedtime relaxes the muscles in your throat, making airway collapse more likely during sleep.
Sleep Position: Your sleeping position significantly impacts breathing during sleep. Back sleeping tends to worsen symptoms as gravity pulls tissues backward, further narrowing the airway.
Physical and Anatomical Factors
Body Structure Issues: Some people are born with anatomical features that increase risk:
- Small or narrow airway
- Enlarged tonsils or adenoids
- Deviated septum
- Large tongue
- Micrognathia (small jaw)
- Low-hanging soft palate
Neck Circumference: A larger neck circumference (greater than 17 inches for men, 16 inches for women) is associated with increased risk due to potential increased soft tissue around the airway.
Age: These conditions become more common as people age, particularly after 40. Muscle tone naturally decreases with age, including in the throat muscles that keep airways open.
Demographic Factors
Gender: Men are 2-3 times more likely to have sleep apnea than premenopausal women. However, women’s risk increases significantly after menopause. Women also tend to experience different symptoms, often reporting insomnia, fatigue, and morning headaches rather than the classic snoring and witnessed apneas.
Family History: Sleep apnea has a genetic component. If family members have the condition, you’re at increased risk.
Medical Conditions
Several health conditions increase sleep apnea risk:
- Heart disease and high blood pressure
- Type 2 diabetes
- Polycystic ovary syndrome (PCOS)
- Pickwickian syndrome (obesity hypoventilation syndrome)
- Previous stroke
- Chronic nasal congestion
- Advanced heart or kidney disease where fluid can build up in the neck
- PTSD
How Are These Conditions Diagnosed?
Since hypopnea involves a reduction rather than total elimination of breathing, it cannot be accurately diagnosed based on symptoms alone. Professional sleep testing is essential for proper diagnosis.
Sleep Studies: The Gold Standard
The most comprehensive diagnostic tool is polysomnography, an overnight sleep study typically conducted in a sleep laboratory. During this test, you’ll be monitored by trained technicians while sensors track:
- Brain waves (electroencephalography/EEG)
- Blood oxygen levels (pulse oximetry)
- Heart rate and rhythm (electrocardiography/ECG)
- Breathing patterns (respiratory effort and airflow)
- Body position during sleep
- Limb movements
- Snoring sounds
- Eye movements (electrooculography)
- Muscle activity (electromyography)
This comprehensive data allows sleep specialists to identify not just whether you have breathing disruptions, but also their type, severity, and relationship to sleep stages and body positions.
At-Home Sleep Testing
For many patients, an at-home sleep apnea test is a convenient and cost-effective alternative. These portable devices monitor fewer parameters than a full polysomnography but can still effectively diagnose obstructive sleep apnea in straightforward cases.
Home tests typically measure:
- Airflow through your nose and mouth
- Breathing effort
- Blood oxygen levels
- Heart rate
- Sometimes body position
However, home tests have limitations. They may underestimate severity, cannot diagnose central sleep apnea, and don’t measure actual sleep time (so AHI calculations are estimates). If your home test is negative but symptoms persist, your doctor may recommend a full sleep study.
Additional Diagnostic Tools
Your healthcare provider may also use:
- Epworth Sleepiness Scale: A questionnaire measuring daytime sleepiness
- STOP-BANG score: A screening tool assessing sleep apnea risk
- Mallampati score: An assessment of oral cavity crowding
- Physical examination: Checking airway anatomy, neck circumference, blood pressure, and body mass index
Comprehensive Treatment Options
The good news is that both hypopnea and sleep apnea are highly treatable conditions. The treatment approach depends on your severity, type of sleep-disordered breathing, anatomy, and personal preferences.
Positive Airway Pressure (PAP) Therapy
CPAP (Continuous Positive Airway Pressure) is the gold standard treatment for moderate to severe obstructive sleep apnea and hypopnea. CPAP machines deliver a steady stream of pressurized air through a mask worn during sleep, creating an “air splint” that keeps your airway open throughout the night.
Modern CPAP therapy has come a long way from the bulky, noisy machines of the past. Today’s devices are:
- Quieter (often under 30 decibels)
- Smaller and travel-friendly
- Equipped with advanced features like ramp settings and pressure relief
- Compatible with various mask types for maximum comfort
The key to CPAP success is finding the right setup for your needs:
- Mask selection: Choose from nasal pillows, nasal masks, or full-face masks
- For side sleepers: Special masks designed to prevent leaks
- For stomach sleepers: Low-profile options
- For mouth breathers: Full-face masks or chin straps
- For bearded users: Masks with better seal technology
BiPAP (Bilevel Positive Airway Pressure) provides two pressure levels—one for inhalation and a lower one for exhalation—making it easier to breathe out against the pressure. BiPAP machines are often used for people who can’t tolerate CPAP or have certain medical conditions.
ASV (Adaptive Servo-Ventilation) is an advanced therapy primarily used for central sleep apnea and complex sleep apnea. ASV machines continuously monitor your breathing and automatically adjust pressure support breath-by-breath.
Lifestyle Modifications
For mild cases and as complementary treatment for all severities, lifestyle changes can be remarkably effective:
Weight Loss: Even modest weight reduction (10% of body weight) can significantly improve or reverse sleep apnea naturally in many overweight individuals. The FDA-approved medication Zepbound has shown promise for treating sleep apnea in people with obesity.
Sleep Position Changes: Positional therapy can reduce symptoms by 50% or more in people with positional sleep apnea. Strategies include specialized pillows, positional alarms, or wearing tennis balls sewn into the back of pajamas.
Avoiding Alcohol and Sedatives: Eliminating these substances, especially within 3-4 hours of bedtime, can reduce airway collapse.
Smoking Cessation: Quitting smoking reduces upper airway inflammation and fluid retention.
Regular Exercise: Physical activity improves muscle tone, aids weight loss, and may directly improve sleep apnea severity even without significant weight loss.
Nasal Congestion Management: Treating chronic nasal obstruction with decongestants, nasal strips, or addressing underlying allergies can improve breathing.
Oral Appliance Therapy
Sleep apnea mouth guards (mandibular advancement devices) are custom-fitted by dentists and work by repositioning your jaw forward during sleep, which keeps the airway open. These devices are:
- Most effective for mild to moderate obstructive sleep apnea
- A good alternative for people who can’t tolerate CPAP
- Portable and convenient for travel
- Silent, which partners appreciate
Surgical Options
When conservative treatments fail or aren’t appropriate, various surgical options can address anatomical obstructions:
Uvulopalatopharyngoplasty (UPPP): Removes excess tissue from the throat to widen the airway.
Tonsillectomy and Adenoidectomy: Particularly effective in children with enlarged tonsils or adenoids causing obstruction.
Hypoglossal Nerve Stimulation: An implanted device (like Inspire therapy) stimulates the nerve controlling tongue movement, preventing it from blocking the airway during sleep.
Maxillomandibular Advancement: A more extensive procedure that repositions the upper and lower jaw forward to enlarge the entire airway.
Nasal Surgery: Corrects structural problems like deviated septum or nasal polyps that contribute to breathing difficulties.
Alternative and Emerging Treatments
Alternative treatments showing varying degrees of promise include:
- Acupuncture: Some studies suggest potential benefits
- Myofunctional therapy: Exercises to strengthen tongue and throat muscles
- EPAP therapy: Small valves worn over the nostrils
- AD109 sleep apnea pill: Investigational medication targeting specific breathing mechanisms
The Serious Health Consequences of Untreated Sleep Apnea
Left untreated, both hypopnea and sleep apnea can lead to severe, life-threatening health complications. The repeated drops in blood oxygen levels and sleep fragmentation trigger a cascade of physiological problems throughout the body.
Cardiovascular Complications
Sleep apnea and cardiovascular health are intimately connected. Untreated sleep apnea significantly increases risk of:
High Blood Pressure (Hypertension): The repeated oxygen drops cause stress hormone surges that elevate blood pressure, even during waking hours. About 50% of people with sleep apnea have hypertension.
Heart Disease: Sleep apnea increases risk of coronary artery disease, heart attacks, and irregular heart rhythms (atrial fibrillation). The repeated oxygen deprivation stresses the heart and blood vessels.
Heart Failure: Sleep apnea is present in 40-50% of people with heart failure and can worsen existing heart failure.
Stroke Risk: Sleep apnea doubles or triples stroke risk. The relationship is bidirectional—sleep apnea increases stroke risk, and stroke can cause or worsen sleep apnea.
Pulmonary Hypertension: Chronic low oxygen levels can lead to high blood pressure in the lungs.
Metabolic Disorders
Untreated sleep apnea disrupts metabolic function:
- Type 2 Diabetes: Sleep apnea impairs glucose metabolism and insulin sensitivity
- Metabolic Syndrome: A cluster of conditions including abdominal obesity, high blood pressure, high blood sugar, and abnormal cholesterol
- Weight Gain: Poor sleep disrupts hormones regulating hunger and satiety, making weight loss extremely difficult
Cognitive and Mental Health Impact
The mental health effects of chronic sleep disruption are profound:
- Depression and Anxiety: Sleep apnea is strongly linked to mood disorders
- Brain Fog: Difficulty concentrating, memory problems, and reduced cognitive performance
- Brain Damage: Chronic oxygen deprivation may cause structural changes in brain regions responsible for memory and thinking
- Increased Risk of Dementia: Long-term untreated sleep apnea may accelerate cognitive decline
Other Serious Complications
Accidents: Sleep deprivation from untreated sleep apnea increases risk of motor vehicle accidents by 2-3 times and workplace accidents.
Seizures: Sleep apnea can lower seizure threshold in people with epilepsy.
Pregnancy Complications: Untreated sleep apnea during pregnancy increases risk of gestational diabetes, preeclampsia, and low birth weight.
Surgical Complications: Sleep apnea increases risks during and after surgery, particularly with anesthesia.
Can You Die from Sleep Apnea?
The sobering answer is yes. While death from sleep apnea during sleep is rare, the condition significantly increases mortality risk through cardiovascular events, accidents, and other complications. Studies show that severe, untreated sleep apnea can increase mortality risk by 40% or more.
Living with Sleep Apnea: Practical Tips for Better Sleep
Receiving a sleep apnea diagnosis can feel overwhelming, but remember: this is a highly treatable condition, and many people live full, healthy lives with sleep apnea once properly treated.
Getting Used to CPAP Therapy
If you’ve been prescribed CPAP, getting used to CPAP therapy takes patience and persistence. Your first night with CPAP may feel strange, but most people adapt within a few weeks. Tips for success:
- Start gradually: Practice wearing the mask during the day while awake
- Use the ramp feature: This starts pressure low and gradually increases
- Overcome CPAP anxiety: Relaxation techniques can help
- Optimize comfort: Try different masks, adjust straps, use CPAP pillows
- Stay consistent: Regular use yields the best results
Managing CPAP Side Effects
Common CPAP challenges and solutions:
- Mask leaks: Ensure proper fit and sizing
- Dry mouth: Use a heated humidifier or full-face mask
- Dry eyes: Adjust mask positioning or try different styles
- Skin irritation: Use mask liners or gentler cleaning products
- Mask marks: Adjust strap tension or try different sleep positions
- Rainout: Condensation in tubing—use heated tubing
- Aerophagia: Swallowing air—may need pressure adjustment
Maintaining Your Equipment
Proper CPAP cleaning and maintenance ensures optimal performance and prevents infections:
- Wash mask daily with mild soap and water
- Clean water chamber daily
- Replace filters according to manufacturer guidelines
- Follow replacement schedules for masks, tubing, and supplies
- Use distilled water in the humidifier
Travel Tips
Don’t let sleep apnea keep you home. With planning, you can travel with CPAP easily:
- Invest in a travel CPAP machine
- Use a CPAP travel bag
- Consider a CPAP battery for camping or areas with unreliable power
- Carry documentation for airport security
Additional Sleep Hygiene Tips
Improve your sleep quality with these strategies:
- Maintain a consistent sleep schedule
- Create a cool, dark, quiet sleep environment
- Avoid large meals within 3 hours of bedtime
- Limit caffeine after 2 PM
- Establish a relaxing bedtime routine
- Consider music for better sleep
Frequently Asked Questions
How do I know if I have sleep apnea or hypopnea?
You cannot self-diagnose these conditions. The only way to definitively distinguish between apnea and hypopnea is through a professional sleep study that measures your breathing patterns throughout the night. If you experience symptoms like chronic snoring, witnessed breathing pauses, or excessive daytime sleepiness, consult your healthcare provider about getting tested.
Can hypopnea become sleep apnea?
While they’re related conditions, hypopnea doesn’t necessarily “progress” to sleep apnea. However, the same risk factors (like weight gain) that worsen hypopnea can also increase the likelihood of full apneas. Many people have both types of events throughout the same night.
Is snoring always a sign of sleep apnea or hypopnea?
Not necessarily. While most people with sleep apnea snore, not all snoring indicates sleep apnea. Simple snoring (primary snoring) without breathing pauses or oxygen desaturations is common and doesn’t require treatment. If you’re concerned, especially if snoring is keeping your partner awake, see a healthcare provider.
How long does CPAP therapy take to work?
Many people notice improvements within the first few nights of CPAP use, including better sleep quality and reduced morning headaches. However, maximum benefits—including improved daytime alertness, better blood pressure control, and enhanced quality of life—typically emerge after several weeks of consistent use. CPAP may even increase life expectancy with long-term adherence.
What if I can’t tolerate CPAP?
Don’t give up! There are many solutions for CPAP intolerance. Work with your healthcare provider to troubleshoot issues, try different mask styles, adjust pressure settings, or explore alternatives like oral appliances, BiPAP, positional therapy, or surgical options.
Can children have hypopnea or sleep apnea?
Yes, sleep apnea can affect children of all ages, though it’s most common in children aged 2-8. Signs include snoring, restless sleep, bedwetting, behavioral problems, and poor school performance. Enlarged tonsils and adenoids are the most common cause in children.
Are women affected differently by sleep apnea?
Yes. Sleep apnea in women often presents differently, with less obvious symptoms like insomnia, morning headaches, fatigue, and depression rather than loud snoring. Women are also diagnosed later and less frequently than men, despite similar health consequences.
What’s the connection between sleep apnea and teeth grinding?
Teeth grinding and sleep apnea often occur together. Some research suggests the grinding may be the body’s attempt to reposition the jaw and reopen the airway during sleep. Treating sleep apnea often reduces teeth grinding.
The Bottom Line: Take Action Today
When I look back at my sleep study results showing 387 breathing disruptions in a single night, I’m grateful I didn’t ignore the warning signs. My journey from severe sleep apnea (with both apneas and hypopneas) to consistent treatment has been life-changing. The afternoon brain fog is gone. My morning headaches disappeared. My energy returned. Most importantly, I’m no longer putting my heart and brain at risk every single night.
Understanding the difference between hypopnea vs sleep apnea is crucial, but what matters most is recognizing that both conditions require professional evaluation and treatment. While hypopnea involves partial airway obstruction and sleep apnea involves complete blockage, both can significantly impact your health, quality of life, and even longevity.
The encouraging news is that modern medicine offers highly effective treatments for these conditions. Whether through CPAP therapy, lifestyle modifications, oral appliances, or surgical interventions, most people can achieve excellent symptom control and dramatically reduce their risk of serious health complications.
If you suspect you might have either condition, don’t wait to seek help. The consequences of untreated sleep-disordered breathing are too serious to ignore, but the benefits of treatment are transformative. A proper diagnosis through a sleep study can identify the problem and allow your healthcare provider to recommend the most effective treatment plan tailored to your specific situation.
Remember, quality sleep isn’t a luxury—it’s a fundamental pillar of health, as essential as nutrition and exercise. Taking action today to address your sleep-disordered breathing can help you wake up feeling refreshed, think more clearly, maintain better cardiovascular health, and enjoy a longer, healthier, more energized life tomorrow.
Don’t let another night of poor sleep rob you of the vitality and well-being you deserve. Talk to your healthcare provider about your symptoms, get tested, and start your journey toward better sleep and better health.
References
- WebMD – Hypopnea: What to Know About This Sleep Disorder
- Cleveland Clinic – Apnea-Hypopnea Index (AHI): What It Is & Ranges
- Medical News Today – Hypopnea: Causes, types, and treatments
- Sleep Foundation – Apnea-Hypopnea Index, Explained
- PMC – The Clinical Significance of Apneas Versus Hypopneas
- Harvard Medical School – Understanding Sleep Study Results
- WebMD – Apnea Hypopnea Index (AHI): Results and Treatment
⚠️ MEDICAL DISCLAIMER This blog provides general information only and is not a substitute for professional medical advice, diagnosis, or treatment. Sleep apnea is a serious condition, and CPAP equipment should be used under proper medical supervision. Always consult your doctor or sleep specialist before starting, stopping, or changing any therapy. I share personal experiences as a CPAP user, not as a medical professional. Individual results vary. For medical guidance, please consult a qualified clinician or the American Academy of Sleep Medicine (aasm.org).