Paroxysmal Nocturnal Dyspnea: Understand this Condition
If you’ve ever woken up in the middle of the night gasping for air, unable to catch your breath, you know how terrifying the experience can be.
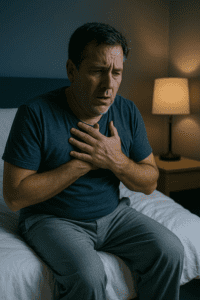
This sudden onset of breathlessness during sleep has a name: Paroxysmal Nocturnal Dyspnea, commonly abbreviated as PND. While it shares some similarities with sleep apnea, PND is a distinct symptom that often signals underlying health conditions requiring medical attention.
In this comprehensive guide, I’ll walk you through everything you need to know about Paroxysmal Nocturnal Dyspnea, including what it is, what causes it, how it differs from sleep apnea, and what treatment options are available.
Medical Disclaimer: The information provided in this article is for educational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. If you experience symptoms of PND, please consult with a qualified healthcare provider for proper evaluation and treatment.
What Is Paroxysmal Nocturnal Dyspnea?
Paroxysmal Nocturnal Dyspnea (pronounced “pair-uh-SIZ-muhl knock-TUR-nuhl DISP-nee-uh”) is a symptom characterized by sudden, severe episodes of shortness of breath that occur during sleep. The term itself provides clues to what’s happening:
- Paroxysmal means the symptoms come on suddenly and may recur
- Nocturnal indicates that symptoms occur at night
- Dyspnea is the medical term for difficult or uncomfortable breathing
According to Cleveland Clinic, PND typically awakens a person from sleep one to two hours after falling asleep. The person wakes up feeling like they can’t catch their breath, often gasping for air and coughing. While frightening, the symptoms usually resolve within 10 to 30 minutes after sitting or standing up.
How PND Feels
People who experience PND describe it in various ways, but common descriptions include:
- A sensation of suffocation or drowning
- Feeling like you can’t get enough air
- Sudden panic upon waking
- An urgent need to sit up or get out of bed
- Gasping or struggling to breathe
- Coughing fits
- Chest tightness or discomfort
Many patients report that sitting upright or standing near an open window provides relief, as the change in position helps alleviate the pressure on the lungs.
PND vs. Sleep Apnea: Understanding the Difference
One of the most common questions people have is whether PND and sleep apnea are the same thing. While both conditions can cause you to wake up gasping for air, they are fundamentally different.
Key Differences
Sleep Apnea is a sleep disorder where breathing repeatedly stops and starts during sleep. There are two main types:
- Obstructive Sleep Apnea (OSA): Physical blockage of the airway causes breathing to stop
- Central Sleep Apnea (CSA): The brain fails to send proper signals to breathing muscles
Paroxysmal Nocturnal Dyspnea is a symptom, not a disorder itself. It’s caused by fluid accumulation in the lungs rather than an airway obstruction or neurological signaling problem.
According to SleepApnea.org, understanding the difference is crucial because PND can indicate a serious heart problem, while sleep apnea is primarily a respiratory issue.
The Connection Between PND and Sleep Apnea
While PND and sleep apnea are different, they can coexist. Research published in the Journal of Cardiology found that respiratory disturbance index (which measures the severity of sleep apnea) was independently associated with a history of PND in patients with heart failure.
Specifically:
- People with severe heart failure may develop central sleep apnea with Cheyne-Stokes respiration, which can present with PND symptoms
- Up to 70% of people with heart failure have sleep-disordered breathing
- About half of those also experience central sleep apnea with Cheyne-Stokes breathing pattern
If you’re experiencing nighttime breathing difficulties, it’s essential to have a proper sleep apnea diagnosis to determine whether you’re dealing with PND, sleep apnea, or both conditions.
What Causes Paroxysmal Nocturnal Dyspnea?
Understanding the underlying mechanisms of PND helps explain why it occurs and who is at risk. The primary cause relates to fluid redistribution in the body when lying down.
The Mechanism Behind PND
When you lie down to sleep, gravity causes blood and fluid to redistribute from your lower extremities and abdomen back toward your chest and lungs. In healthy individuals, the heart efficiently pumps this extra blood volume through the circulatory system without issue.
However, when the heart is weakened or diseased, it cannot adequately handle this increased blood volume. As explained by the National Center for Biotechnology Information (NCBI), this failure results in:
- Pulmonary congestion (fluid buildup in the lungs)
- Decreased vital capacity
- Reduced pulmonary compliance
- Accumulation of fluid in the alveoli (air sacs) and lung tissue
The result is the sensation of breathlessness that characterizes PND.
Common Underlying Causes
1. Congestive Heart Failure (CHF)
Heart failure is the most common cause of PND. According to WebMD, when the heart muscle struggles to pump blood adequately throughout the body, fluid builds up in and around the lungs (pulmonary edema), making breathing difficult.
PND specifically occurs with left-sided heart failure, where the left ventricle fails to pump blood effectively. The connection between heart failure and breathing difficulties extends to other symptoms as well, including sleep apnea and cardiovascular health complications.
2. Coronary Artery Disease
Coronary artery disease reduces blood supply to the heart muscle, weakening the heart’s pumping ability. This contributes to heart failure and, consequently, PND. The reduced blood flow means the heart cannot effectively manage the redistribution of fluid that occurs when lying down.
3. Heart Valve Disorders
Malfunctioning heart valves impair blood flow through the heart chambers. When valves don’t open or close properly, blood can back up into the lungs, causing fluid accumulation and triggering PND episodes.
4. Hypertension (High Blood Pressure)
Uncontrolled high blood pressure puts excessive strain on the heart over time. This chronic stress can lead to heart failure and increase the risk of PND. Managing blood pressure is crucial for preventing cardiovascular complications.
5. Chronic Obstructive Pulmonary Disease (COPD)
COPD and other chronic lung conditions can cause PND by impairing lung function. When lung capacity is already compromised, the additional fluid redistribution that occurs when lying down can overwhelm the respiratory system.
6. Asthma
Healthline notes that asthma symptoms often worsen at night. When the lungs become congested with fluid, people with asthma may experience attacks that present as PND. Severe asthma also increases the risk of developing obstructive sleep apnea, further elevating PND risk.
7. Central Sleep Apnea with Cheyne-Stokes Breathing
This specific pattern of breathing, commonly seen in people with heart failure, can cause PND. The American Academy of Sleep Medicine recommends CPAP therapy and nocturnal oxygen therapy for this condition.
8. Pulmonary Hypertension
Sleep apnea and pulmonary hypertension often occur together. Pulmonary hypertension (high blood pressure in the lungs) can contribute to right-sided heart failure and PND symptoms.
9. Obesity
While obesity doesn’t directly cause PND, it significantly worsens the condition. Excess abdominal fat adds pressure to the diaphragm and chest cavity, making breathing more difficult when lying down. Obesity is also a major risk factor for both sleep apnea and heart disease.
10. Kidney Disease
Kidney problems can lead to fluid retention throughout the body, including the lungs. This excess fluid exacerbates PND symptoms, especially in people with concurrent heart conditions.
Risk Factors for Paroxysmal Nocturnal Dyspnea
According to Wikipedia’s medical documentation, common risk factors for PND include:
Cardiac Risk Factors:
- High blood pressure
- High cholesterol
- Diabetes
- Obesity
- Sedentary lifestyle
- Poor diet
- Family history of heart disease
- Advanced age (over 60)
- Male gender
Pulmonary Risk Factors:
- Tobacco use (including secondhand smoke and sleep apnea)
- Exposure to air pollution
- Occupational exposure to hazardous fumes
- History of lung infections or diseases
- Allergen sensitivity
Other Risk Factors:
- Pregnancy (PND during pregnancy is abnormal and requires immediate medical evaluation)
- Alcohol abuse
- Recreational drug use (particularly cocaine)
- History of heart transplant rejection
Symptoms and Associated Conditions
While sudden breathlessness is the hallmark symptom of PND, several other symptoms often accompany it:
Primary Symptoms:
- Sudden onset of severe breathlessness during sleep
- Coughing that may be dry or produce frothy sputum
- Wheezing or bronchospasm similar to asthma (sometimes called “cardiac asthma”)
- Chest tightness or discomfort
- Rapid, shallow breathing (tachypnea)
- Use of accessory respiratory muscles (visible effort in neck and chest muscles)
Associated Symptoms:
- Orthopnea: Breathlessness when lying flat (differs from PND as it occurs while awake)
- Leg swelling (edema) due to fluid retention
- Fatigue and weakness
- Weight gain from fluid retention
- Nighttime urination (nocturia)
- Daytime breathlessness with minimal exertion
- Mental confusion or altered mental status (in severe cases)
- Anxiety or fear related to breathing difficulties
Warning Signs of Medical Emergency
According to Cleveland Clinic, seek immediate medical attention if PND is accompanied by:
- Low blood pressure
- Significantly decreased respiratory rate
- Altered mental status or confusion
- Hypoxia (low blood oxygen levels)
- Cyanosis (blue tint to lips or skin)
- Stridor (high-pitched breathing sound)
- Unstable heart rhythms (arrhythmias)
- Severe or prolonged chest pain
- Symptoms that don’t improve with sitting upright
These symptoms may indicate acute heart failure, pulmonary edema, or other life-threatening conditions requiring emergency care.
Diagnosis: How Doctors Identify PND
Diagnosing PND involves identifying both the symptom itself and the underlying cause. Healthcare providers use multiple approaches to reach an accurate diagnosis.
Medical History and Physical Examination
The diagnostic process begins with a thorough evaluation:
- Symptom description: When do episodes occur? How long do they last? What provides relief?
- Medical history: Existing heart or lung conditions, medications, lifestyle factors
- Physical examination: Listening to heart and lung sounds, checking for edema, assessing breathing patterns
- Risk factor assessment: Evaluating cardiac and pulmonary risk factors
Your doctor will ask detailed questions about your sleep apnea symptoms and breathing patterns to differentiate PND from other conditions.
Diagnostic Tests
Depending on the suspected underlying cause, your healthcare provider may order:
Cardiac Tests:
- Echocardiogram: Ultrasound imaging of the heart to assess:
- Heart chamber size and function
- Pumping efficiency (ejection fraction)
- Valve function
- Fluid around the heart
- Electrocardiogram (ECG/EKG): Records electrical activity to detect:
- Irregular heart rhythms
- Previous heart attacks
- Heart muscle thickening
- Conduction abnormalities
- Cardiac MRI: Provides detailed images of heart structure and function
- Coronary Angiogram: Visualizes blood flow through coronary arteries to detect blockages
- Cardiac Stress Test: Evaluates heart function during physical exertion
- Myocardial Biopsy: In rare cases, tissue samples help diagnose specific heart conditions
Blood Tests:
- B-type Natriuretic Peptide (BNP) or NT-proBNP: Elevated levels indicate heart failure
- Cardiac troponins: Detect heart muscle damage
- Complete blood count (CBC): Screens for anemia and infection
- Electrolyte panel: Checks sodium, potassium, and other electrolyte levels
- Kidney function tests: Assess fluid balance regulation
- Thyroid function tests: Rule out thyroid-related heart problems
Pulmonary Tests:
- Chest X-ray: Reveals:
- Fluid in the lungs (pulmonary edema)
- Heart size and shape
- Lung conditions like pneumonia or COPD
- Chest CT Scan: Provides detailed lung images to identify:
- Structural abnormalities
- Blood clots
- Lung disease
- Pulmonary Function Tests: Measure lung capacity and airflow
- Pulse Oximetry: Monitors blood oxygen levels
Sleep Studies:
As noted by the Sleep Foundation, polysomnography (sleep study) may be necessary to:
- Diagnose coexisting sleep apnea
- Differentiate PND from other sleep-related breathing disorders
- Identify Cheyne-Stokes respiration patterns
- Measure oxygen levels during sleep
- Assess sleep quality and disruption
At-home sleep apnea testing options are also available for initial screening, though more complex cases may require in-lab studies.
Treatment Options for Paroxysmal Nocturnal Dyspnea
Treatment for PND focuses on addressing the underlying cause while managing symptoms to improve quality of life. The approach is multifaceted and individualized based on the specific condition causing PND.
Medications
For Heart Failure:
- Diuretics: Help remove excess fluid from the body
- Reduce pulmonary congestion
- Decrease workload on the heart
- Common examples: furosemide (Lasix), bumetanide
- ACE Inhibitors: Improve heart function and reduce blood pressure
- Relax blood vessels
- Decrease fluid retention
- Examples: lisinopril, enalapril
- Beta-Blockers: Slow heart rate and reduce blood pressure
- Decrease heart workload
- Improve cardiac output
- Examples: carvedilol, metoprolol
- Angiotensin Receptor Blockers (ARBs): Alternative to ACE inhibitors with similar benefits
- Aldosterone Antagonists: Additional diuretic effect and heart protection
For Respiratory Conditions:
- Bronchodilators: Relax airway muscles
- Inhaled medications for asthma and COPD
- Improve airflow
- Corticosteroids: Reduce inflammation in airways
- Oral or inhaled forms
- Manage chronic lung conditions
- Antibiotics: Treat underlying pneumonia or respiratory infections
For Hypertension:
- Calcium channel blockers
- Additional ACE inhibitors or ARBs
- Combination medications as needed
Positive Airway Pressure Therapy
For PND related to sleep apnea or heart failure with sleep-disordered breathing:
CPAP Therapy
Continuous Positive Airway Pressure machines deliver constant air pressure to keep airways open. According to treatment guidelines, CPAP for central sleep apnea with Cheyne-Stokes breathing can significantly improve PND symptoms.
Benefits include:
- Prevention of airway collapse
- Improved oxygenation
- Reduced cardiac stress
- Better sleep quality
For those new to CPAP, understanding how to get used to CPAP therapy and preparing for your first night with CPAP can ease the transition.
BiPAP Therapy
Bilevel Positive Airway Pressure provides two pressure levels:
- Higher pressure during inhalation
- Lower pressure during exhalation
- May be more comfortable for some patients
Understanding the difference between APAP, BiPAP, and CPAP helps determine which therapy is most appropriate.
ASV Therapy
Adaptive Servo-Ventilation is specifically designed for complex sleep apnea and central sleep apnea:
- Automatically adjusts pressure levels
- Responds to breathing patterns
- Particularly effective for Cheyne-Stokes respiration
Learn more about how ASV works and ASV machines to understand this advanced treatment option.
Oxygen Therapy
Supplemental oxygen may be prescribed:
- For temporary use during acute episodes
- As ongoing treatment for chronic conditions
- Often combined with positive airway pressure therapy
- Improves blood oxygen levels
- Reduces strain on the heart and lungs
Surgical Interventions
When medications and non-invasive treatments aren’t sufficient:
Cardiac Procedures:
- Coronary Artery Bypass Grafting (CABG): Restores blood flow to heart muscle
- Angioplasty and Stenting: Opens blocked coronary arteries
- Valve Repair or Replacement: Corrects malfunctioning heart valves
- Implantable Devices:
- Implantable cardioverter-defibrillators (ICDs)
- Cardiac resynchronization therapy (CRT) devices
- Pacemakers
- Heart Transplant: For severe, treatment-resistant heart failure
Other Procedures:
- Hypoglossal Nerve Stimulation for Obstructive Sleep Apnea
- Inspire Treatment as an alternative to CPAP
- Sleep apnea surgery options for anatomical obstructions
- Uvulopalatopharyngoplasty to remove excess throat tissue
Lifestyle Modifications
Lifestyle changes play a crucial role in managing PND:
Diet:
- Reduce sodium intake: Helps minimize fluid retention
- Follow a heart-healthy diet: Mediterranean-style eating patterns
- Limit caffeine and alcohol: Especially before bedtime
- Stay hydrated: But avoid excessive fluids before bed
- Maintain healthy weight: Reduces cardiac and respiratory strain
CPAP therapy and weight loss often go hand in hand, as improved sleep can support weight management efforts.
Physical Activity:
- Regular, moderate exercise strengthens the heart and lungs
- Walking, swimming, or cycling as tolerated
- Consult a healthcare provider for an appropriate exercise plan
- Pulmonary rehabilitation for lung conditions
- Cardiac rehabilitation for heart patients
Sleep Positioning:
- Elevate head and upper body: Use multiple pillows or an adjustable bed
- Sleep on your side: May reduce fluid accumulation
- Best sleeping position for sleep apnea can help minimize symptoms
- Positional therapy may be beneficial
Sleep Hygiene:
- Maintain consistent sleep schedule
- Create comfortable sleep environment
- Manage stress through relaxation techniques
- Avoid late-evening large meals
- How to sleep better with sleep apnea offers additional strategies
Substance Avoidance:
- Quit smoking (or never start)
- Limit alcohol consumption
- Avoid recreational drugs
- Be cautious with sedating medications
Weight Management:
- Achieve and maintain healthy BMI
- Even modest weight loss can significantly improve symptoms
- Consider medical weight management programs if needed
- Emerging treatments like Zepbound for sleep apnea show promise
Stress Management:
- Practice relaxation techniques
- Consider cognitive behavioral therapy
- Mindfulness meditation
- Support groups for chronic illness
Monitoring and Follow-Up
Regular medical monitoring is essential:
- Periodic echocardiograms to assess heart function
- Blood pressure monitoring
- Weight tracking (rapid weight gain may indicate fluid retention)
- Medication adjustments as needed
- Sleep study follow-ups to assess treatment effectiveness
Living with Paroxysmal Nocturnal Dyspnea
While PND can be frightening and disruptive, many people successfully manage the condition with proper treatment and lifestyle modifications.
Coping Strategies
- Keep medications accessible: Have prescribed medications readily available
- Prepare your sleeping area:
- Extra pillows for elevation
- Easy access to light switches
- Keep a glass of water nearby
- Communicate with family: Ensure household members understand your condition and know when to seek emergency help
- Track symptoms: Keep a log of episodes, including:
- Time of occurrence
- Duration
- Severity
- Potential triggers
- What provided relief
- Manage anxiety: PND episodes can cause significant anxiety about sleep. Consider:
- Relaxation techniques before bed
- Cognitive behavioral therapy
- Professional counseling if anxiety becomes overwhelming
- Stay informed: Understanding your condition empowers you to manage it effectively
Impact on Quality of Life
PND significantly affects daily life:
- Sleep disruption: Leading to sleep deprivation and daytime fatigue
- Physical limitations: Reduced exercise tolerance
- Emotional impact: Anxiety, depression, and fear
- Social effects: May impact relationships and work
However, with proper treatment, many patients experience substantial improvement in symptoms and quality of life.
When to Seek Emergency Care
Call 911 or seek immediate medical attention if:
- PND symptoms don’t improve after sitting up
- Severe chest pain accompanies breathing difficulty
- You experience extreme confusion or altered mental status
- Breathing becomes extremely difficult
- Lips or skin turn blue (cyanosis)
- You feel like you’re going to pass out
- Symptoms are much worse than previous episodes
Special Populations
Pregnancy and PND
PND during pregnancy is considered abnormal and requires immediate medical evaluation. While some shortness of breath is normal during pregnancy due to:
- Increased oxygen demands
- Pressure from growing uterus
- Hormonal changes
True PND suggests a serious cardiac condition requiring urgent assessment to protect both mother and baby.
Children and PND
PND can occur in children, though it’s less common than in adults. In pediatric cases, causes may include:
- Congenital heart defects
- Severe asthma
- Sleep apnea in children
- Pneumonia or other respiratory infections
Does my child have sleep apnea provides guidance on recognizing breathing problems in young people.
Elderly Patients
Older adults face a higher PND risk due to:
- Increased prevalence of heart disease
- Multiple concurrent health conditions
- Reduced physiological reserves
- Medication interactions
Careful management and close monitoring are essential in this population.
The Connection Between PND and Related Conditions
Understanding how PND relates to other health issues provides important context:
PND and Overlap Syndrome
Overlap syndrome—the coexistence of COPD and obstructive sleep apnea—can significantly increase PND risk due to compounded effects on the respiratory and cardiovascular systems.
PND and Complex Sleep Apnea
Complex or mixed sleep apnea combines features of both obstructive and central sleep apnea, making PND more likely and treatment more challenging.
PND and Cardiovascular Complications
PND often occurs alongside other cardiovascular symptoms:
- Increased stroke risk
- Erectile dysfunction
- Mental health effects, including PTSD connections
Cognitive Function and PND
The combination of disturbed sleep and reduced oxygenation can lead to:
- Brain fog with CPAP therapy improvements
- Potential brain damage from untreated sleep apnea
- Memory problems and cognitive decline
Prognosis and Long-Term Outlook
The outlook for PND depends heavily on the underlying cause and how well it’s managed.
Factors Affecting Prognosis:
Positive Factors:
- Early diagnosis and treatment
- Good medication compliance
- Successful lifestyle modifications
- Effective management of underlying conditions
- Access to appropriate medical care
Challenging Factors:
- Severe heart failure
- Multiple comorbidities
- Advanced age
- Poor treatment adherence
- Delayed diagnosis
Heart Failure Prognosis
For PND caused by heart failure:
- Five-year survival rates vary widely depending on severity
- Modern treatments have significantly improved outcomes
- Early intervention is crucial
- Does CPAP increase life expectancy discusses how treating sleep-disordered breathing can improve cardiac outcomes
Other Causes
For PND due to:
- Asthma: Generally good prognosis with proper management
- COPD: Progressive disease requiring ongoing treatment
- Sleep apnea: Excellent prognosis with effective therapy
- Treatable cardiac conditions: Variable but often favorable with appropriate intervention
Emerging Research and Future Treatments
Medical research continues to advance our understanding and treatment of PND:
Current Research Areas:
- Biomarkers: Identifying blood markers that predict PND episodes
- Advanced Imaging: Better visualization of cardiac and pulmonary function
- Personalized Medicine: Tailoring treatments to individual patient characteristics
- Novel Medications: New drug therapies targeting specific mechanisms
- Technology Integration: Wearable devices for monitoring and early warning
Promising Developments:
- Future of ASV technology: More sophisticated adaptive ventilation
- AD109 sleep apnea pill: Pharmacological alternatives to PAP therapy
- Telemedicine: Remote monitoring and management
- AI-powered diagnostics: Earlier and more accurate identification of at-risk patients
Prevention: Reducing Your Risk
While not all cases of PND can be prevented, you can significantly reduce your risk:
Primary Prevention:
- Maintain cardiovascular health:
- Control blood pressure
- Manage cholesterol
- Prevent or manage diabetes
- Maintain healthy weight
- Protect lung health:
- Don’t smoke
- Avoid air pollution when possible
- Treat respiratory infections promptly
- Use protective equipment in hazardous environments
- Live a heart-healthy lifestyle:
- Regular physical activity
- Balanced, nutritious diet
- Stress management
- Adequate sleep
- Limit alcohol
- Avoid recreational drugs
Secondary Prevention:
For those with existing risk factors or early heart disease:
- Regular medical checkups: Early detection and treatment
- Medication compliance: Take prescribed medications as directed
- Symptom monitoring: Report new or worsening symptoms promptly
- Disease management: Control chronic conditions effectively
- Sleep apnea treatment: Address sleep-disordered breathing
Frequently Asked Questions
Is PND the same as a panic attack?
No. While both can cause sudden breathlessness and anxiety, PND is caused by fluid in the lungs from underlying medical conditions, while panic attacks are psychiatric episodes without physical lung or heart disease causing the breathlessness.
Can I die from PND?
PND itself is a symptom, not a direct cause of death. However, the underlying conditions causing PND—particularly severe heart failure or acute pulmonary edema—can be life-threatening if untreated. This is why medical evaluation is crucial.
How quickly should I see a doctor after experiencing PND?
You should contact your healthcare provider as soon as possible after your first episode. If symptoms are severe, don’t improve with sitting up, or are accompanied by chest pain or other warning signs, seek emergency care immediately.
Can PND be cured?
PND can often be eliminated or significantly reduced by successfully treating the underlying cause. For example, effectively managing heart failure with medications and lifestyle changes can prevent PND episodes. However, if the underlying condition is chronic and progressive, ongoing management rather than “cure” may be more realistic.
Do I need a sleep study if I have PND?
Your doctor may recommend a sleep study to:
- Rule out or confirm coexisting sleep apnea
- Identify specific breathing patterns like Cheyne-Stokes respiration
- Determine optimal treatment approaches
- Monitor treatment effectiveness
How is PND different from orthopnea?
Orthopnea is breathlessness that occurs immediately when lying down and is relieved by sitting up—it happens while you’re awake. PND occurs after you’ve been asleep for 1-2 hours and wakes you from sleep. Both can indicate heart failure but have slightly different mechanisms.
Can losing weight eliminate PND?
Weight loss can significantly improve or eliminate PND if obesity is a contributing factor. Excess weight, particularly abdominal fat, increases strain on both the heart and lungs. Even modest weight loss (5-10% of body weight) can make a substantial difference.
Will I need to use CPAP forever?
If CPAP is prescribed for sleep apnea contributing to PND, you may need to use it long-term. However, if you make significant lifestyle changes (such as substantial weight loss), your need for CPAP might decrease or resolve. Never discontinue CPAP without consulting your healthcare provider.
Conclusion
Paroxysmal Nocturnal Dyspnea is a serious symptom that should never be ignored. While experiencing sudden breathlessness during sleep can be frightening, understanding what’s happening and seeking appropriate medical care can lead to effective management and significantly improved quality of life.
The key points to remember:
- PND is a symptom, not a disease: It indicates an underlying condition, most commonly heart failure, that requires treatment
- Early medical evaluation is crucial: Don’t wait to see a doctor if you experience episodes of waking up gasping for air
- Treatment focuses on the underlying cause: Managing heart failure, lung disease, or sleep apnea can eliminate or greatly reduce PND episodes
- Lifestyle modifications matter: Diet, exercise, weight management, and avoiding harmful substances all play important roles
- Multiple treatment approaches exist: From medications to CPAP therapy to surgical interventions, effective options are available
- Quality of life can improve significantly: With proper treatment and management, many patients experience substantial symptom reduction
If you’re experiencing symptoms of PND or have concerns about your nighttime breathing, don’t hesitate to reach out to a healthcare provider. Early intervention can prevent serious complications and help you return to restful, restorative sleep.
Remember, this article is for informational purposes only and should not replace professional medical advice. Every individual’s situation is unique, and treatment should be tailored to your specific needs under the guidance of qualified healthcare professionals.
Related Reading:
- What Is Sleep Apnea?
- Obstructive Sleep Apnea
- Central Sleep Apnea
- Sleep Apnea Symptoms
- Sleep Apnea and Cardiovascular Health
- Living with Sleep Apnea
About This Article: This comprehensive guide on Paroxysmal Nocturnal Dyspnea was researched using information from reputable medical sources, including the Cleveland Clinic, the National Center for Biotechnology Information, Sleep Foundation, Healthline, WebMD, and peer-reviewed medical journals. For specific questions about your health, always consult with a qualified healthcare provider.
References and Medical Sources
- Cleveland Clinic – “Paroxysmal Nocturnal Dyspnea (PND): Causes & Treatment” – https://my.clevelandclinic.org/health/symptoms/paroxysmal-nocturnal-dyspnea
- National Center for Biotechnology Information (NCBI) – “Dyspnea, Orthopnea, and Paroxysmal Nocturnal Dyspnea – Clinical Methods” – https://www.ncbi.nlm.nih.gov/books/NBK213/
- Healthline – “Paroxysmal Nocturnal Dyspnea Causes and Treatment” – https://www.healthline.com/health/paroxysmal-nocturnal-dyspnea
- Sleep Foundation – “Paroxysmal Nocturnal Dyspnea” – https://www.sleepfoundation.org/sleep-apnea/paroxysmal-nocturnal-dyspnea
- WebMD – “What Is Paroxysmal Nocturnal Dyspnea (PND)?” – https://www.webmd.com/sleep-disorders/what-is-paroxysmal-nocturnal-dyspnea
- SleepApnea.org – “Understanding Paroxysmal Nocturnal Dyspnea” – https://www.sleepapnea.org/paroxysmal-nocturnal-dyspnea/
- Journal of Cardiology – “Association between sleep apnea and overnight hemodynamic changes in hospitalized heart failure patients with and without paroxysmal nocturnal dyspnea” – https://www.journal-of-cardiology.com/article/S0914-5087(13)00037-3/fulltext
- Wikipedia – “Paroxysmal nocturnal dyspnoea” (Medical Documentation) – https://en.wikipedia.org/wiki/Paroxysmal_nocturnal_dyspnoea
- ScienceDirect Topics – “Paroxysmal Nocturnal Dyspnoea – an overview” – https://www.sciencedirect.com/topics/medicine-and-dentistry/paroxysmal-nocturnal-dyspnoea
- Allure Medical – “Paroxysmal Nocturnal Dyspnea” – https://www.alluremedical.com/paroxysmal-nocturnal-dyspnea/
- PubMed/NCBI – “Association between sleep apnea and overnight hemodynamic changes in hospitalized heart failure patients with and without paroxysmal nocturnal dyspnea” – https://pubmed.ncbi.nlm.nih.gov/23507270/
Medical Review Note: Information in this article is sourced from peer-reviewed medical literature, academic medical centers, and reputable health organizations. Last reviewed: November 2025.
⚠️ MEDICAL DISCLAIMER This blog provides general information only and is not a substitute for professional medical advice, diagnosis, or treatment. Sleep apnea is a serious condition, and CPAP equipment should be used under proper medical supervision. Always consult your doctor or sleep specialist before starting, stopping, or changing any therapy. I share personal experiences as a CPAP user, not as a medical professional. Individual results vary. For medical guidance, please consult a qualified clinician or the American Academy of Sleep Medicine (aasm.org).