Sleep Apnea and COVID-19 Risks: Precautions and Tips
Jeremy Smith is a long-term CPAP user and sleep apnea advocate. After being diagnosed with severe obstructive sleep apnea, he created ByJeremySmith.com to help others navigate CPAP therapy through personal stories, gear reviews, and practical advice.
Sleep Apnea and COVID-19. Is there a connection?
Since the COVID-19 pandemic began, evidence suggests people with certain health conditions may face increased COVID-19 and sleep apnea risks.
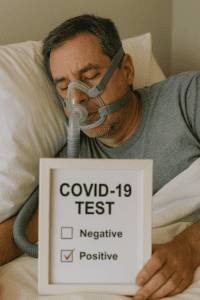
Sleep apnea, a condition that disrupts breathing during sleep, can amplify respiratory health concerns and potential complications with COVID-19.
Understanding this sleep apnea COVID-19 connection can help those affected take appropriate precautions and maintain optimal health.
For me, I have probably always had severe apnea, but I was diagnosed 10 years ago. I have had COVID-19 twice, so as mine is already severe, I can’t tell if COVID has made it more severe!
In this article, we’ll explore how sleep apnea might increase the risk of severe COVID-19 outcomes, how the pandemic impacts those with sleep apnea, and proactive steps you can take to manage your health.
1. Understanding Sleep Apnea
Sleep apnea is a common yet often underdiagnosed sleep disorder. The most prevalent form, obstructive sleep apnea (OSA), occurs when throat muscles relax excessively during sleep, blocking airflow.
Central sleep apnea (CSA), a less common form, results from the brain not sending proper signals to the muscles controlling breathing.
Both types have symptoms, including loud snoring, episodes of breathing cessation, morning headaches, daytime fatigue, and, in severe cases, cardiovascular issues.
2. COVID-19 and Respiratory Health Risks with Sleep Apnea
COVID-19 primarily impacts the respiratory system, causing symptoms that range from mild (cough, fever, and shortness of breath) to severe (pneumonia and acute respiratory distress syndrome).
Since COVID-19 and sleep apnea both affect respiratory health, people with sleep apnea may face a higher risk of complications.
The sleep apnea COVID-19 connection may include factors like reduced immune response, cardiovascular health, and impaired breathing during sleep.
2.1 How Sleep Apnea Impacts Immune Response with COVID-19
Research shows poor sleep quality, often present in sleep apnea patients, can impair the immune system.
Those with sleep apnea experience repeated interruptions in breathing, which lower oxygen levels and cause the body to release stress hormones.
This stress response can weaken immunity, making it harder to combat infections and creating additional sleep apnea immune response COVID-19 risks.
2.2 Increased Risk of Cardiovascular Complications
COVID-19 affects cardiovascular health, leading to inflammation and blood clotting issues.
Because sleep apnea is linked to higher risks of cardiovascular disease, combining these with COVID-19 and sleep apnea may heighten health risks.
People with obstructive sleep apnea are at increased risk for hypertension, heart disease, and stroke—all complications that can also arise or worsen with COVID-19.
3. Why People with Sleep Apnea May Be at Higher Risk for Severe COVID-19 Complications
3.1 Breathing Difficulties During Sleep
Since both COVID-19 and sleep apnea impact breathing, patients with sleep apnea may experience more severe symptoms if they contract COVID-19.
Lower oxygen levels during sleep apnea episodes combined with COVID-19-related breathing issues can lead to prolonged symptoms, including low oxygen levels and a longer recovery.
3.2 Increased Inflammation and the Role of CPAP Therapy
People with sleep apnea often have higher levels of systemic inflammation. Since COVID-19 can also trigger severe inflammatory responses, the sleep apnea COVID-19 connection suggests that combining the two conditions may lead to complications.
Many people with sleep apnea rely on Continuous Positive Airway Pressure (CPAP) therapy to maintain open airways during sleep. This therapy can potentially reduce inflammation and stabilize breathing, even for those experiencing mild COVID-19 symptoms.
4. Should People with Sleep Apnea Take Extra COVID-19 Precautions?
While COVID-19 vaccines provide substantial protection, individuals with sleep apnea and COVID-19 risks should take extra steps to protect their health. Here’s what experts recommend:
4.1 Maintain CPAP Therapy Diligently
Using CPAP consistently is critical for managing sleep apnea, especially during a pandemic. Regular CPAP use can reduce daytime fatigue, stabilize blood pressure, and improve respiratory function.
If you experience COVID-19 symptoms, consult your healthcare provider to discuss CPAP use and any needed adjustments, as proper CPAP use and COVID-19 safety is essential.
4.2 Follow Basic COVID-19 Protocols
While it might seem repetitive, wearing masks, washing hands frequently, and avoiding crowded indoor spaces are highly effective in reducing virus exposure, helping you mitigate COVID-19 and sleep apnea connection risks.
4.3 Vaccination and Boosters
COVID-19 vaccinations and boosters are effective in reducing the risk of severe outcomes, including hospitalization and death. Staying up-to-date with vaccines is especially important for people with respiratory conditions like sleep apnea.
5. CPAP Therapy and COVID-19 Safety: Precautions and Best Practices
Since CPAP devices emit a steady airflow, some have raised concerns about their use spreading viral particles in shared spaces. Here’s how to manage CPAP use and COVID-19 safety effectively:
5.1 Isolate If Possible
If you share a room or live with others, consider isolating in a separate room while using your CPAP. This minimizes the risk of spreading airborne particles.
5.2 Maintain Strict Hygiene
Disinfect your CPAP machine, mask, and tubing regularly. Use CPAP-specific disinfecting products or mild soapy water, and avoid alcohol-based cleaners that can degrade equipment over time.
5.3 Monitor Symptoms Closely
While using CPAP therapy, track your symptoms carefully. Contact your healthcare provider promptly if you experience increased shortness of breath, chest pain, or abnormal fatigue.
6. Research Findings on Sleep Apnea COVID-19 Complications
Multiple studies have linked sleep apnea to more severe COVID-19 outcomes, although ongoing research continues to examine this COVID-19 and sleep apnea connection. For example:
- A study in JAMA Network Open found that people with sleep apnea who contracted COVID-19 were more likely to experience severe symptoms and require hospitalization.
- Research from the American Academy of Sleep Medicine suggests that untreated sleep apnea may exacerbate COVID-19 respiratory complications, especially in patients with risk factors like obesity or diabetes.
7. How Sleep Apnea Patients Can Stay Informed and Supported
COVID-19 and sleep apnea are evolving study areas, so staying informed is essential. Here are some ways to keep up with the latest research:
- Regular Check-Ins with Your Doctor: Maintain communication with your healthcare provider, especially if you notice changes in your health.
- Online Communities: Many people find support in online forums like Reddit where they can share advice, experiences, and tips for managing sleep apnea COVID-19 risks.
- Follow Reputable Sources: For trustworthy updates, stick to reliable health sources, such as the Centers for Disease Control and Prevention (CDC) and the American Academy of Sleep Medicine.
8. Practical Tips for Managing Sleep Apnea and COVID
Here are a few more actionable tips to help you manage sleep apnea and COVID-19 risks effectively:
8.1 Prioritize Healthy Sleep Habits
Getting quality sleep can strengthen your immune system. Follow sleep hygiene practices, such as keeping a consistent bedtime, avoiding heavy meals late at night, and limiting screen exposure an hour before bed.
8.2 Maintain a Healthy Diet
A balanced diet rich in vitamins and minerals can help your body recover from the effects of poor sleep. Include foods high in antioxidants and omega-3 fatty acids, which may support respiratory and immune health.
8.3 Reduce Stress Through Relaxation Techniques
Chronic stress can worsen both sleep apnea symptoms and immune response. Practice relaxation techniques like deep breathing exercises or meditation to manage stress and boost mental health.
9. Does Sleep Apnea Cause Long COVID?
While research on the link between sleep apnea and long COVID is ongoing, some potential connections exist.
Sleep apnea can contribute to chronic inflammation and reduced immune function, both of which may increase vulnerability to prolonged COVID-19 symptoms, known as long COVID.
People with sleep apnea who contract COVID-19 might experience worsened fatigue, respiratory issues, and other long COVID symptoms due to pre-existing respiratory strain and reduced oxygen levels.
Ongoing studies aim to clarify whether sleep apnea patients are more likely to develop long COVID.
Conclusion
Managing sleep apnea during COVID-19 may require additional precautions for those with sleep apnea, but these efforts are worthwhile.
By staying informed, using CPAP therapy responsibly, and adhering to health guidelines, you can reduce sleep apnea COVID-19 risks and maintain a healthier lifestyle despite the challenges posed by COVID-19.
Sleep apnea may increase vulnerability to respiratory illnesses, but with the right strategies, you can protect yourself and continue managing your health effectively.
For more tips on living well with sleep apnea, check out resources on byjeremysmith.com.
Disclaimer: The content on this blog is for informational and educational purposes only and is not a substitute for professional medical advice. Always speak with your doctor or sleep specialist before starting, stopping, or changing any treatment or therapy related to sleep apnea or CPAP use.